Researchers led by Prof Giovanna Mallucci from UK DRI at Cambridge, have shown that modulation of a pathway involved in the production of cellular proteins is a potentially safe and viable therapy for dementia. The proof-of-concept study, published today (11 August) in the journal Science Signaling, unlocks opportunities to develop drugs targeting this pathway, which is often disrupted in people with neurodegenerative diseases.
The ‘unfolded protein response’ is an essential biological mechanism that maintains healthy protein levels and function of cells. Research has shown that in neurodegenerative diseases, build-up of pathological proteins causes stress to neurons and leads to the chronic overactivation of the unfolded protein response. Specifically, sustained activation of two components, PERK and eIF2a, leads to a drop in the production of proteins which causes synapses to fail and eventual loss of neurons.
Researchers including Prof Mallucci have had great success in showing that therapeutics can be used to stop this neurodegeneration in animal models, however, serious side effects such as toxicity to the pancreas have been observed, as the normal function of PERK and eIF2a are compromised in other healthy cells and organs. The group therefore set about finding ways to target this pathway that wouldn’t provoke these unwanted secondary effects.
This is exciting proof-of-principle that there are safe ways to modulate this important pathway for the treatment of neurodegenerative diseaseProf Giovanna MallucciCentre Director at UK DRI at Cambridge
The team began by looking at how PERK activates eIF2a and found that modulation of an amino acid in PERK (phosphorylation of Thr799) may have potential in disrupting the two proteins at their interaction site. After confirmation that this did occur in cells, and the activity of eIF2a had been suppressed, the group turned to mice with prion disease as a model of neurodegeneration. By administering a compound to the mice which increased phosphorylation of Thr799, they found that this reduced activity of eIF2a, stopped neuronal loss and increased mouse survival – all without the side effect of damage to the pancreas.
On the findings, Lead author Dr Daniel Hughes, said:
“Our study shows that we can specifically fine-tune PERK-eIF2a signalling in a way that is both neuroprotective and does not cause toxicity in other organs. The long-term aim is to find safe drugs which can achieve this in people living with neurodegenerative diseases.”
The authors noted that while the compound administered to the mice with prion disease did protect neurons, it was used only to show that the correct pathways are being targeted as a proof of principle. Further work will involve fine tuning this modulation and exploring whether the results can be translated into the clinic in future.
Reference:
Targeting the kinase insert loop of PERK selectively modulates PERK signaling without systemic toxicity in mice
By Daniel T. Hughes, Mark Halliday, Heather L. Smith, Nicholas C. Verity, Colin Molloy, Helois Radford, Adrian J. Butcher, Giovanna R. Mallucci
SCIENCE SIGNALING 11 AUG 2020
Article published: 11 August 2020
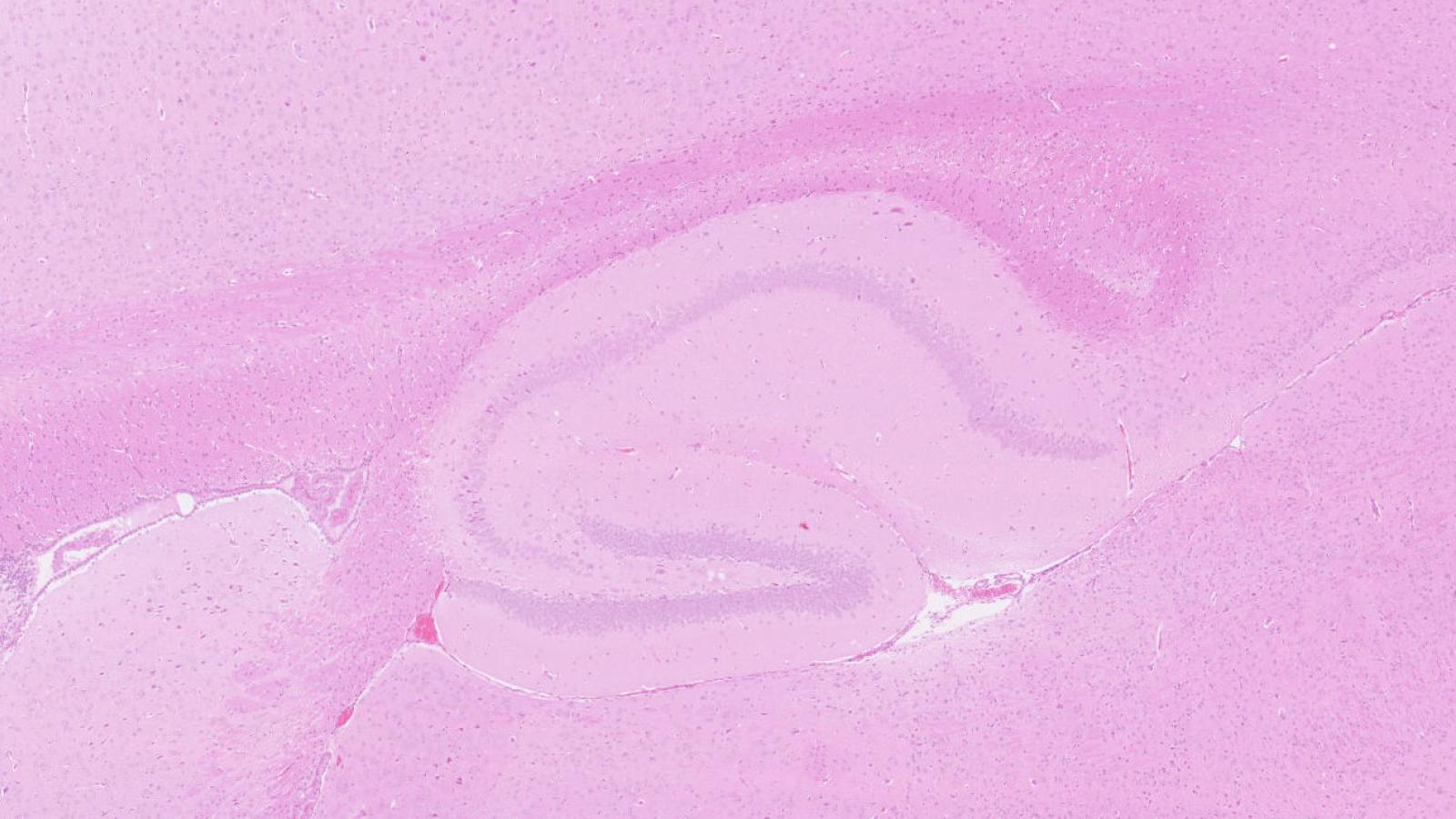
Banner image of hippocampus from healthy mouse, courtesy of the Mallucci Lab