What is motor neuron disease/ALS?
Motor neuron disease (MND) is the general name that’s given to a group of illnesses which can affect nerves called motor neurons in the brain and spinal cord. The most common subtype of MND is amyotrophic lateral sclerosis (ALS), which is also often the most widely used term in other countries. Other names include Maladie de Charcot and Lou Gehrig’s disease.
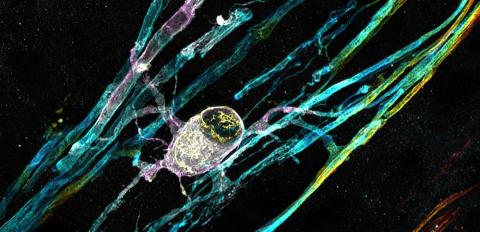
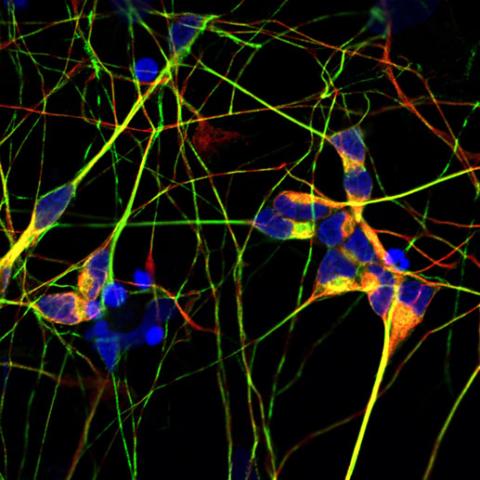
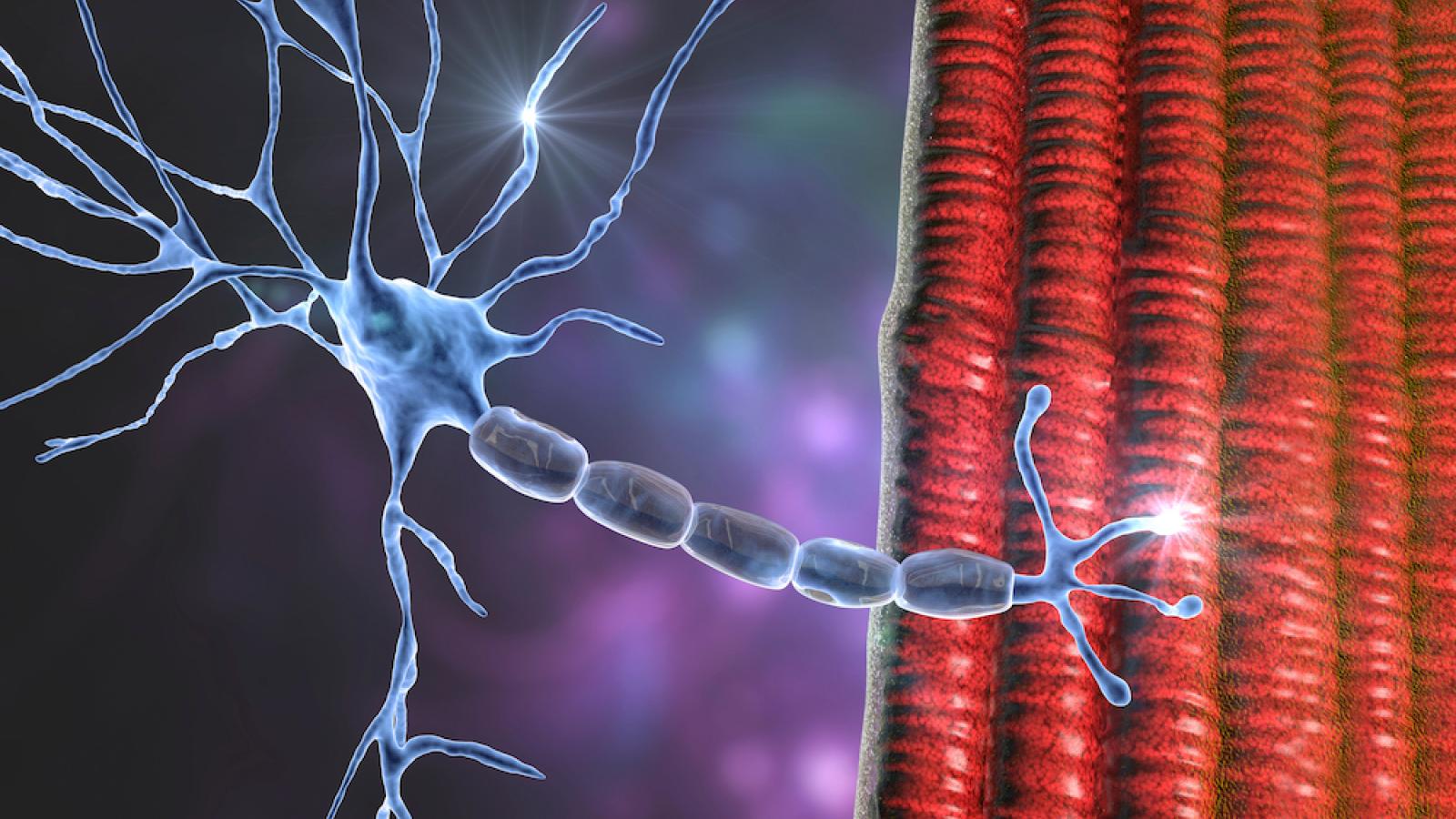
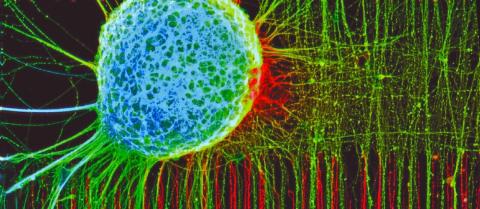
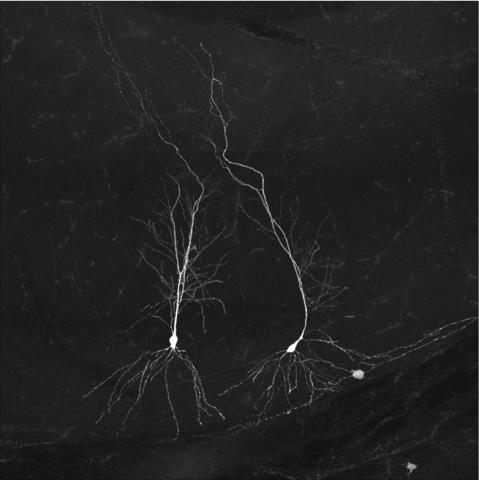
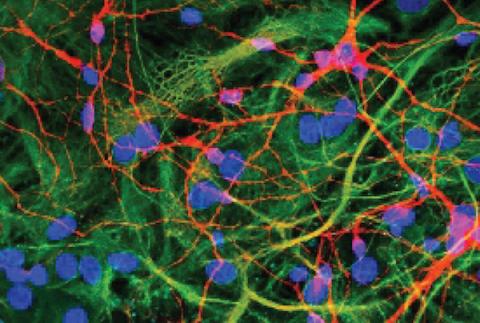
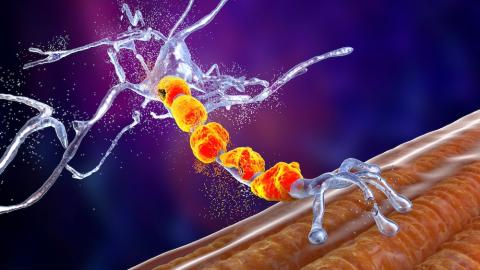
Motor neurons carry signals from the brain and spinal cord directly to the muscles to tell them what to do. In people living with MND/ALS, the disease can prevent these signals from reaching the muscles. This can lead to muscle weakness and may cause stiffness and cramping. The condition can also affect movement, speech, breathing and the ability to swallow.
MND/ALS is a progressive, life-limiting illness. However, symptoms can be managed to enable people living with the condition to maintain a good quality of life.

The innovative MND-SMART clinical trial brings together people involved in the studies. Credit: Maverick Photo Agency.
UK DRI is unlocking transformative treatments
At the UK DRI, our commitment to improving the lives of people living with MND/ALS has been unwavering since our inception, with our many teams across the UK driving breakthroughs from fundamental discoveries to clinical trials. In this article, we discuss the latest breakthroughs, and how UK DRI scientists are charging a pivotal moment in MND/ALS research.
Frequently asked questions
- How common is motor neuron disease/ALS?
It’s estimated that MND affects around 5,000 adults in the UK at any one time. The MND Association estimates that six people are diagnosed with the disease every day in the UK1.
The most common subtype of MND is amyotrophic lateral sclerosis (ALS), which contributes approximately 90% of cases2.
- What are the symptoms of motor neuron disease/ALS?
There are many different symptoms associated with MND/ALS, and many of them can also occur as a result of other health conditions or short-term lifestyle factors such as illness and not sleeping well.
Some of the initial symptoms of MND/ALS can include:
- Tripping: When a muscle gets weaker, it can reduce in size. This is known as muscle wasting. If the muscles in the feet, ankles or legs become weaker, this can increase the risk of tripping or falling. With MND/ALS, ‘foot drop’ can be an early symptom where one foot will sometimes feel weak or drag. However, foot drop could also be due to an injury or another condition.
- Difficulty holding and gripping items: Weakness in the hands and tending to drop things or finding it harder to grip may indicate a neurological problem. However, these symptoms can also be caused simply by getting older, or they could be due to joint problems such as arthritis or to a trapped nerve, so this symptom alone might be nothing to worry about.
- Muscle twitching: People living with MND/ALS may experience a twitching or rippling sensation under their skin. Twitching as a symptom of progressive MND/ALS could affect just one area of the body or several areas simultaneously. Tiredness, stress, having a viral infection and going through a period of ill health can also cause muscles to twitch. Twitching is usually only associated with MND/ALS when other symptoms are also present.
- Fatigue or extreme tiredness: As with muscle twitching, while fatigue can be a symptom of MND/ALS, if it is one of the only symptoms, it’s more likely to be due to another cause. As the disease progresses, it can make people feel very tired and lethargic.
People with MND/ALS have their own individual experience of the condition, and these symptoms may occur at different times during the disease progression. There is more information about the symptoms of MND/ALS on the MND Association’s website. Other useful sources of information include MND Scotland, the ALS Association and My Name’5 Doddy.
- How is motor neuron disease/ALS diagnosed?
If you or someone you care about is experiencing symptoms of motor neuron disease/ALS, please contact a GP for an accurate diagnosis and to rule out other conditions.
There is no single diagnostic test for MND/ALS; instead, diagnosis is based on a combination of clinical history and a medical examination. Various tests such as electromyography or nerve conduction may also be carried out.
Electromyography (EMG) is a type of diagnostic test that’s used to assess the health of muscles and the nerve cells (or motor neurons) that control them. Nerve conduction is another test that’s similar to EMG but measures how quickly the nerves can create an electrical signal.
There are also other tests that can be carried out, including magnetic resonance imaging (MRI) scanning of the brain and spinal cord.
If you are at all worried about your own or a loved one’s health, chatting through your concerns with your GP is an important first step. They may want to monitor how the symptoms progress over many weeks or months. Keeping a symptoms diary can be a useful way of keeping track of what’s happening and can be helpful in making an accurate diagnosis.
- What treatments are there for motor neuron disease/ALS?
Although MND/ALS is a progressive, life-limiting illness, there are treatments available to help with symptom relief. A multidisciplinary team of healthcare professionals will work together to provide a range of care services for people living with the condition.
Healthcare professionals that could be involved in MND/ALS care include neurologists, respiratory specialists, physiotherapists, dietitians, and speech and language therapists. As the disease progresses, additional support from a palliative care nurse may also be needed.
Symptom treatment can come in a range of forms to help improve quality of life for people living with the condition. For example:
- Physiotherapy can be very helpful with relieving muscle cramps. In some cases, a medication called quinine could also be prescribed.
- Muscle stiffness (also known as spasticity) can be treated using medication such as baclofen, which helps to relax muscles.
- For people who experience communication difficulties as a result of MND/ALS, speech and language therapy can help with teaching techniques to make speech as clear as possible.
- MND/ALS can also cause difficulties with eating and drinking. In this case, dieticians can provide advice and support on adapting diet and managing nutrition appropriately.
Other symptomatic medications including tizanidine, dantrolene or gabapentin may also be used to treat muscle problems associated with MND/ALS. In the UK, healthcare professionals follow national guidelines which list a range of treatments and interventions that have been studied and shown to be beneficial in relieving symptoms for people living with MND/ALS.
The only medication currently licensed as a treatment for MND/ALS in the UK is riluzole. It is thought to slow down the damage to the motor neuron cells by reducing their sensitivity to the nerve transmitter glutamate. It can extend survival in advanced cases by a few short months.
People who are prescribed riluzole will need to have blood tests for the first few months to check their liver is functioning properly.
There is more information about what to expect in terms of treatment and the NHS care journey on the MND Association’s website.
- How can I get involved in research and trials for motor neuron disease/ALS?
MND/ALS is an important area of research and at any given time there are a number of trials actively recruiting volunteers to take part. The following websites include links and useful information about getting involved in research:
- Support for motor neuron disease/ALS
Support is crucial, not only for those living with motor neuron disease/ALS, but also for their families and carers. For more information about support available, visit our page on ‘support for people affected’.
The team from UK DRI at King’s have launched a new podcast ‘Between the signals’ aimed at bringing greater understanding about neurodegenerative conditions, and the groundbreaking research going into treating them, to a public audience. In the first episode ‘What is motor neuron disease?’ they discuss common symptoms, diagnosis and current treatments for the condition. The episode coincided with Global MND Awareness Day which falls on 21 June.
What are the causes of motor neuron disease/ALS?
The causes of motor neurone disease/ALS are not yet fully known, although researchers worldwide are trying to learn more about what triggers the disease.
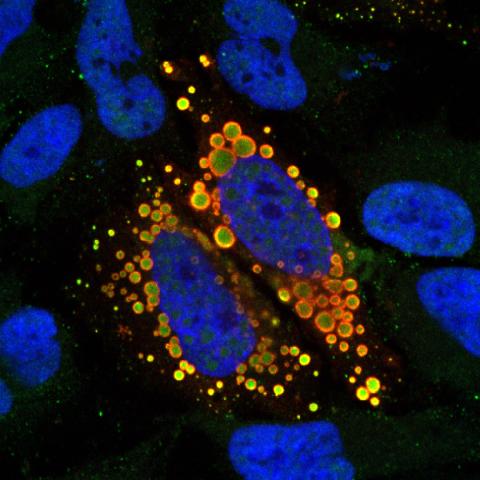
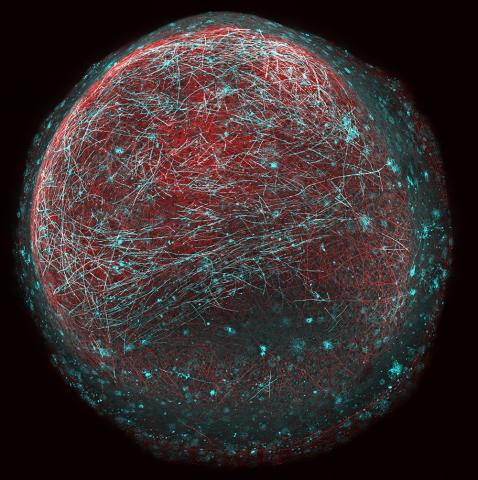
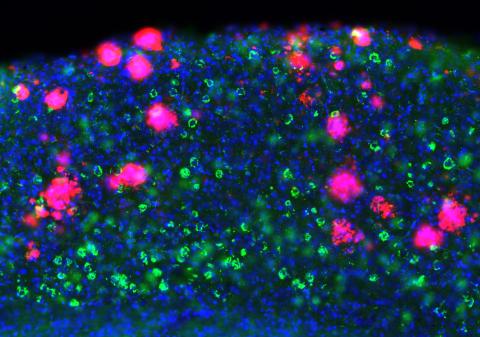
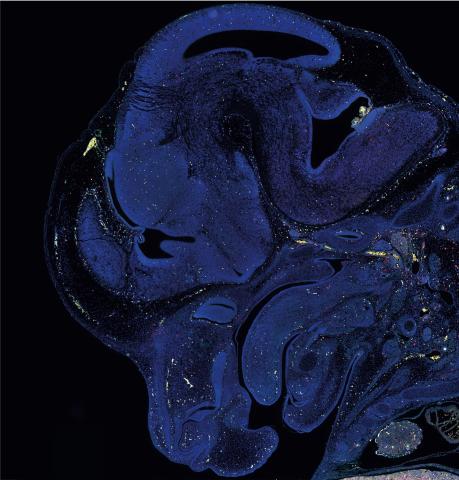
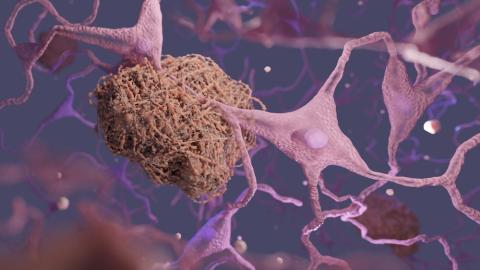
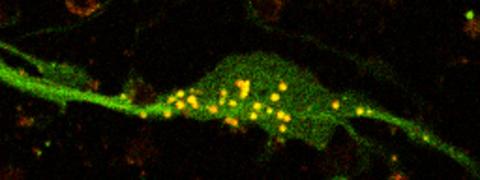
Similar to other neurodegenerative conditions, the build-up of harmful protein – in most cases TDP-43 – is a key hallmark and is likely to contribute to the degeneration of motor neurons.
For most people with MND/ALS, certain genes appear to have some impact on the onset of the disease. For around 1 in 10 people with the condition, genes play a much larger role. ‘Inherited MND/ALS’ is when a family history of MND/ALS increases the level of risk for other family members3.
There are also environmental factors which have been investigated as potential links, including exposure to certain chemicals and high levels of exercise.
Current thinking about what causes MND/ALS indicates that a number of genetic, environmental and lifestyle risk factors may need to combine before most forms of the disease develop. It’s thought that together, these risk factors could tip the balance towards someone developing MND/ALS. At the UK DRI, our researchers are tackling the causes of MND/ALS from multiple angles, with expert investigators working on both laboratory-based research projects and clinical trials.
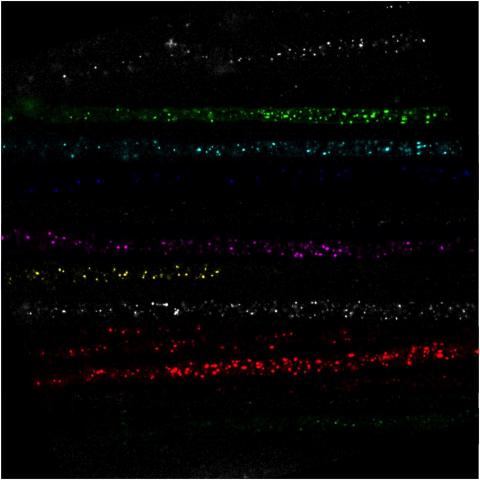
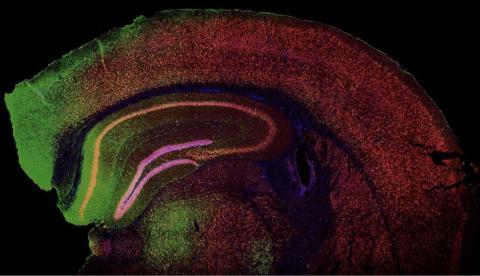
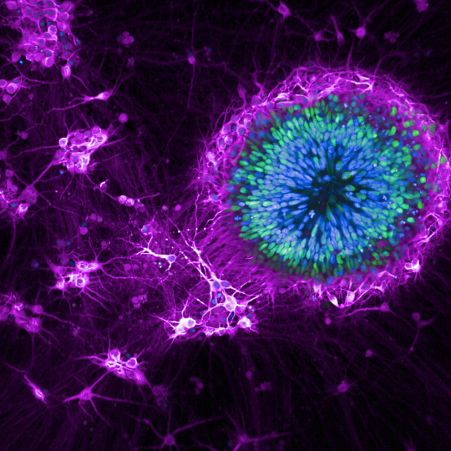
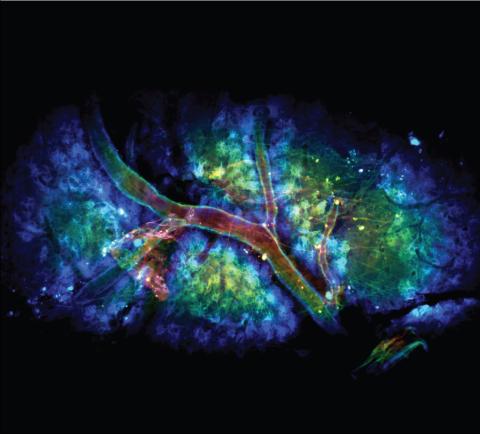
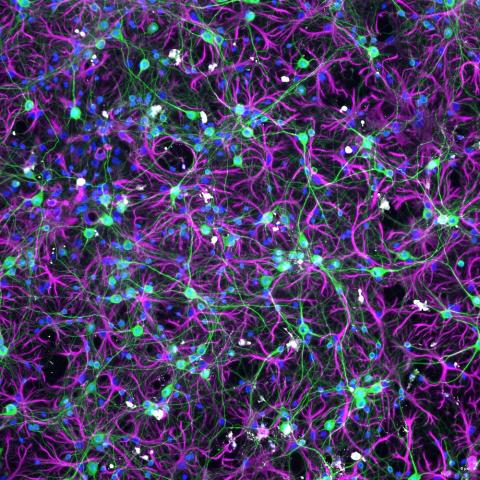
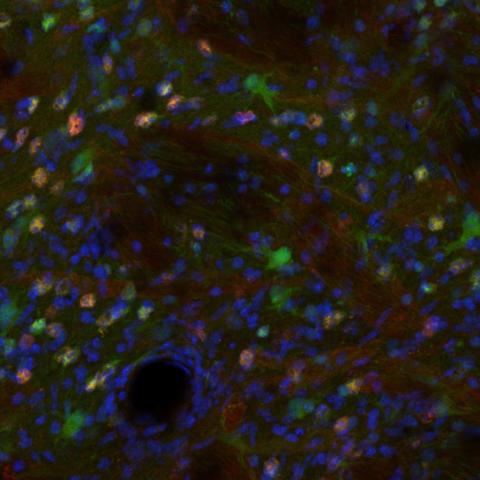
The discovery that MND/ALS and frontotemporal dementia, diseases with distinct clinical symptoms, share the most common genetic cause – a faulty C9orf72 gene – has helped build our knowledge of both conditions. New research models are being harnessed to better understand the molecular and cellular drivers, including how abnormal TDP-43 contributes to progression of the diseases. Several of our lab teams study MND/ALS and frontotemporal dementia in parallel to help build knowledge of both conditions.
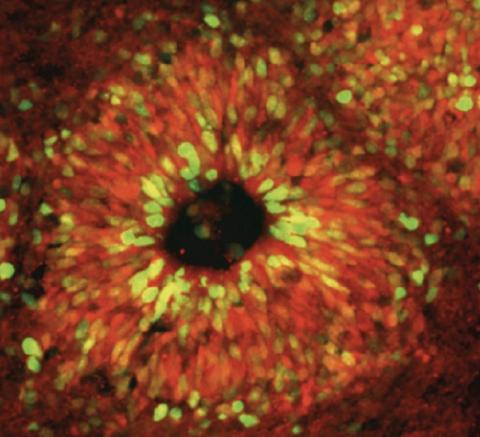
We are also at the forefront of emerging research that can make a difference to people living with MND/ALS, both now and in the future, and invest in several initiatives aimed at accelerating the delivery of treatments to those affected by MND/ALS. These include gene therapy trials for MND/ALS and frontotemporal dementia which are currently being carried out by AviadoBio, a UK DRI at King’s College London spin-out company.
In addition, UK DRI’s Director Prof Siddharthan Chandran and UK DRI Co-investigator Prof Suvankar Pal are leading a pioneering MND-SMART clinical trial platform – currently the largest MND trial in the UK with 800 people at 22 sites in all four nations. This enables several combinations of existing drugs to be tested simultaneously to reduce the duration of trials and increase the chances of effective treatments being approved for MND/ALS.
The UK DRI at King's centre focuses on studying the molecular causes and looking for treatments for motor neuron disease and frontotemporal dementia. In this video, Centre Director Jernej Ule, Group Leader Sarah Marzi, and Centre Manager Tanisha Lewis explain the centre’s research and why they are proud to be part of the UK DRI at King’s.
Latest news


Labs working on motor neuron disease/ALS