Researchers led by Prof Siddharthan Chandran, Group Leader at UK DRI at Edinburgh, have created millimetre-wide 3D organoids from human stem cells. The new model provides a promising new platform for studying neurological diseases and testing drugs for conditions including multiple sclerosis (MS).
The body of a neuron, the axon, carries electrical messages, allowing communication in our nervous system. These electrical impulses can travel at speeds up to 120 metres per second due to a fatty insulating axonal coat called myelin. However, in a number of neurological conditions including MS – an incurable disease affecting more than 100,000 people in the UK – the myelin is damaged which leads to a wide range of devastating symptoms, including mobility issues, fatigue and vision problems.
people are affected by multiple sclerosis in the UK
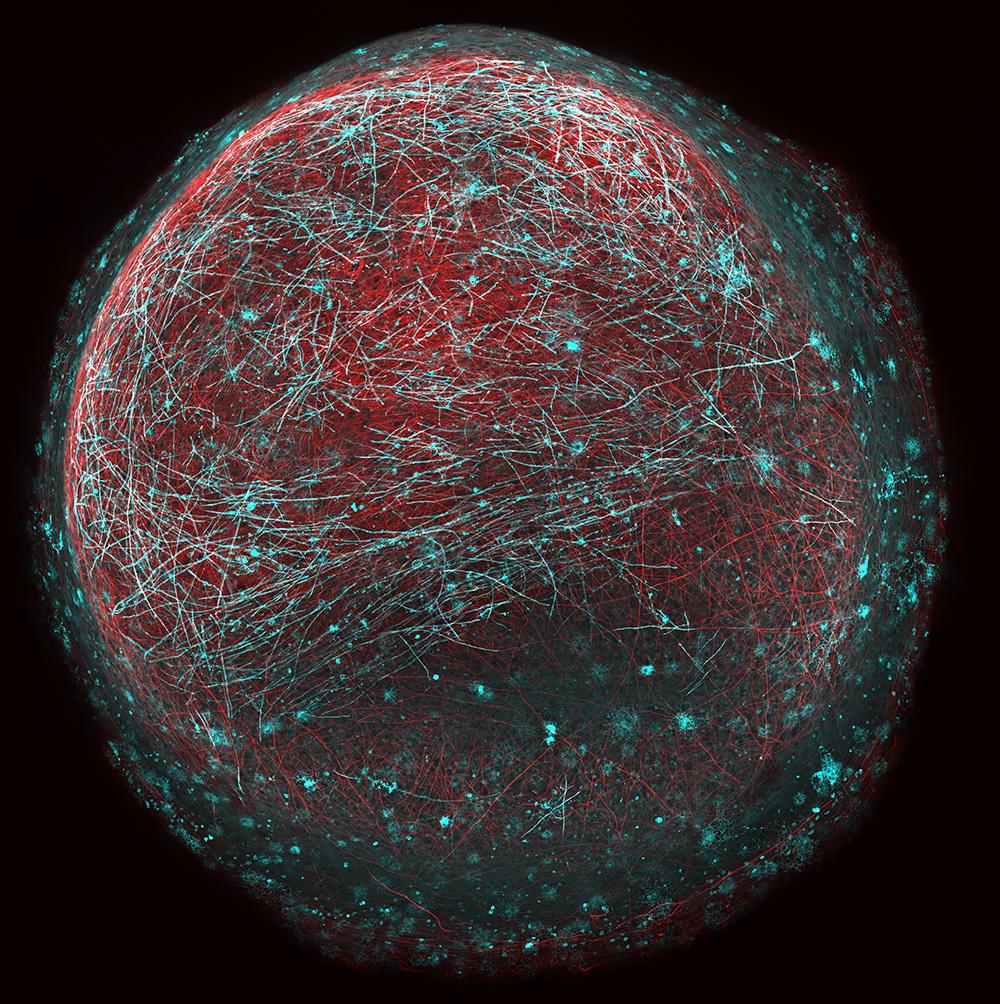
Human stem cell-derived 'mini brain' containing neurons (red) being wrapped in specialised 'myelin' insulation (blue). Each mini brain is 1-2mm in diameter. This model can
Studying neurological disorders like MS represents a huge challenge due to problems accessing brain and spinal cord tissue without risk and huge inconvenience to patients. Using animal models can overcome some issues, however, they can be also be limited in how well they reflect human disease and the way that drugs interact with human cells. In this new study published in the scientific journal Developmental Cell, the research team based at the Anne Rowling Regenerative Neurology Clinic and the Euan MacDonald Centre for Motor Neuron Disease Research, set about developing a human myelin model using skin samples donated by volunteers.
Skin cells were reprogrammed into induced pluripotent stem cells (iPSCs), which can be turned into other cell types – in this case – spinal cord cells. These cells were then grown slowly into organoids – 3-D structures of cell bundles including neurons and distinctive brain cells known as oligodendrocytes that are key to creating myelin. Crucially, the researchers were able to see myelin developing spontaneously around the axons between cells within the organoids. By looking at the axons under a microscope, they could see that the myelin in this model was functioning as it would in a healthy brain or spinal cord.
Now we have the capability of studying human myelination experimentally, a major goal is to identify drugs that can promote myelination.Dr Owen Gwydion JamesLead researcher
The research team then created an organoid using stem cells from a patient with a rare gene mutation that affects myelination. The model showed that key aspects of this cell bundle were consistent with the disease. These new models will allow scientists to compare the differences between the cells of healthy individuals and those with different neurological diseases and to test drugs of interest in human cells before using them in a full clinical trial with patients.
Lead researcher, Dr Owen Gwydion James, said:
“Demyelinating disorders have a profound effect on the quality of life for patients. Now we have the capability of studying human myelination experimentally, a major goal is to identify drugs that can promote myelination. We believe that this new approach could be a huge boost to the toolbox that allows us to do this effectively.”
The authors added that the model is a significant step forward in the study of human myelination and drug development, but caution that treatments tested on this model are still some way from being offered to patients.
The study was funded by the Euan MacDonald Centre and carried out in collaboration with the UK DRI and the MS Society Centre for MS Research at the University of Edinburgh.
Reference
Article published: 20 May 2021
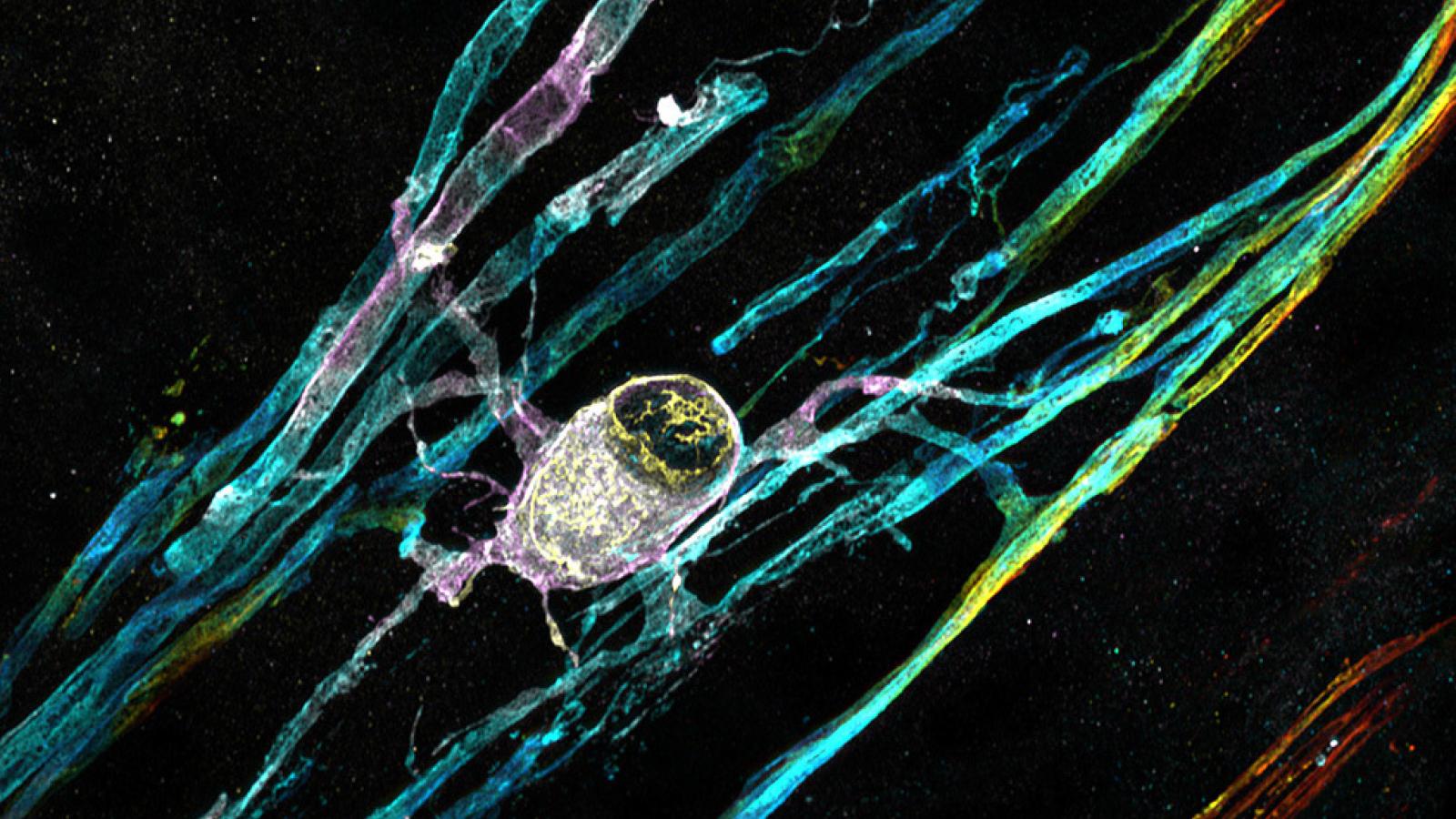
Banner image: Human stem cell-derived myelinating oligodendrocyte can be seen with many myelinating processes wrapped around unstained neurons.
In-line image: Myelin moon
Both images courtesy of Dr Owen Gwydion James, Prof Siddharthan Chandran’s Lab, UK DRI at Edinburgh.