A research team led by Dr Jing Qiu and Prof Giles Hardingham from the UK DRI at Edinburgh, has identified key signals sent between cells to maintain a healthy microenvironment in the brain. The findings will improve current brain research methods and point to new strategies to counteract harmful changes seen in ageing and neurodegenerative disease.
The brain contains a diverse population of cells that work together to maintain healthy function. One specialised immune cell type, microglia, surveys the brain environment, targeting damage and injury to tissue. However, when studied outside of the body, microglia change shape and adopt inflammatory characteristics similar to those seen during ageing or in neurodegenerative disease. These observations suggest signals within the brain’s microenvironment are crucial in maintaining healthy microglia, but questions remain as to what these key signalling cues are and which cell types they come from.
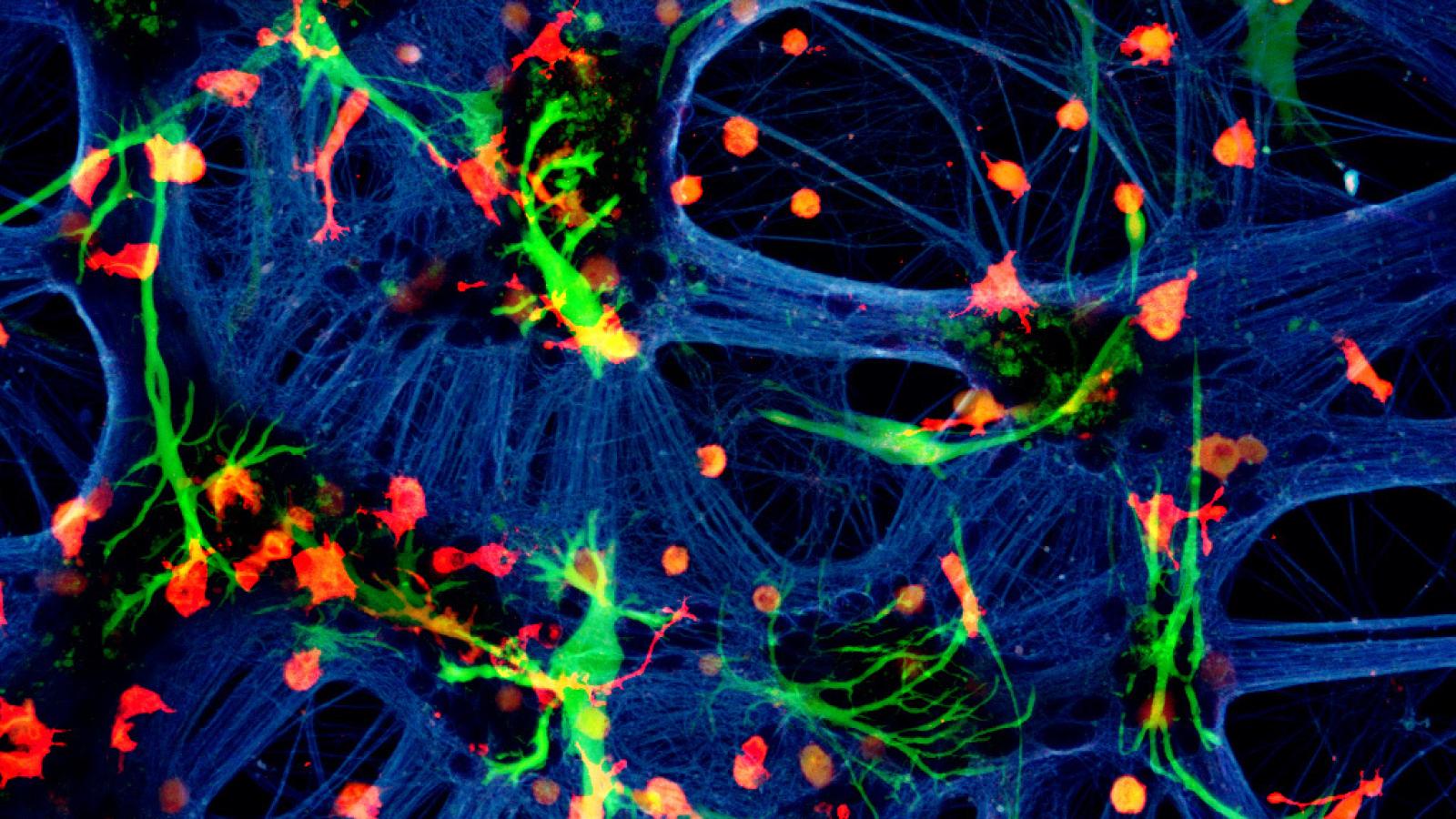
In a new study published today in the scientific journal Cell Reports, a team led by Dr Jing Qiu, took neurones, microglia and astrocytes (another glial cell found in the brain) from different species and cultured them together in the same dish. By exploiting small differences in DNA sequence between the species, changes in gene expression in all cell types could be identified by a computer programme, without the need to physically sort the cells - a method pioneered by UK DRI at Edinburgh. The researchers found evidence that neurones and astrocytes cooperate to maintain healthy microglia, indicated by a branched cell shape and the expression of genes ordinarily lost when microglia are in isolation, aged or diseased.
“When microglia are cultured in isolation, gene expression associated with homeostasis is lost while we see an increase in gene expression associated with infection and injury. It is interesting that both neurones and astrocytes are required to reverse these trends, highlighting the positive impact these cell types are having in the brain,” said study co-lead, Dr Jing Qiu.
To begin pinpointing the signalling pathways involved, the team used protein mass spectrometry to identify molecules that may be involved from the liquid surrounding the cells. They then applied a series of inhibitors to show that a secreted factor known as TGF-β2 was important in this process.
The findings help explain why microglial inflammatory profile changes so markedly when the cells are studied outside of the body.Prof Giles HardinghamStudy co-lead and Centre Director (UK DRI at Edinburgh)
Finally, the researchers wanted to know if neurones and astrocytes were altering the response of the microglia to an inflammatory stimulus, in this case bacterial lipopolysaccharide (LPS). They found that isolated microglia were not in a chronic dysregulated state but rather primed and ready to react to stimulus with an exaggerated response. This primed microglial state is thought to be important in the harmful neuroinflammation seen in several neurodegenerative diseases and these findings suggest that neurones and astrocytes work together to suppress that.
On the implications of the study, Prof Giles Hardingham, co-lead and Centre Director (UK DRI at Edinburgh), said:
“The findings help explain why microglial inflammatory profile changes so markedly when the cells are studied outside of the body. In addition to providing a useful research platform for studying microglia, we now have a greater understanding of the cells and factors important in maintaining a healthy homeostatic environment in the brain, and strategies to counter detrimental effects in ageing and disease.”
To develop these investigations further, Dr Qiu was recently awarded a £250,000 Neuroimmunology Data Generation Award from the Medical Research Council to identify novel factors, therapeutic targets and drugs that are able to restore the microglia to a healthy homeostatic state, prevent age and disease-associated changes, and thus limit harmful neuroinflammation.
Reference
Article published: 23 March 2021
Banner Image: A mixed species co-culture with mouse neurones (blue – beta-tubulin), human astrocytes (green – GFAP) and rat microglia (red – Iba1) courtesy of Dr Paul Baxter