Over the past decade, advances in genetic technology have allowed scientists to investigate human disease at an unprecedented level, bringing the prospect of new and effective treatments closer than ever before. One researcher taking advantage of these new opportunities is Dr Nathan Skene, Group Leader at UK DRI at Imperial, who is using cutting-edge genetic and statistical approaches to gain greater understanding of the cell types responsible for dementia. We caught up with Nathan to find out more about his research, how genetics is revolutionising our understanding of disease and his hope for treatments in the future.
“What I'm really trying to do is to answer simple questions about brain diseases. The most fundamental of these questions is where in the brain does this disease occur? The way that I see complex diseases, such as Alzheimer's or Parkinson's, is that they are driven by a particular cell type/s in the brain and that is where the disease occurs.
While the brain is a complex system and, in the process of the disease many different aspects will become involved, I think that there is a fundamental pathway, a thing that has gone wrong and that will have a place in the brain. With Alzheimer's, we can see that it's more or less an 80% genetic disease. So, if we understand where the genetics act, then we understand what the disease is, and where it is.”
Based on these principles, Dr Skene, who has a background in computational biology, develops statistical methods to pull together data by probing active genes in the mouse nervous system and from large-scale human genetic studies. This groundbreaking work allows researchers to identify where the disease is most likely to originate, and which cell types can be targeted for therapeutics. In his most recent publication, Nathan and his collaborators used this method to discover that Parkinson’s was not only associated with the cells most predominantly lost in the disease, dopaminergic neurons, but also brain support cells known as oligodendrocytes and enteric neurons found in the gut.
“The next step is to know at which time point in the development of that cell does the genetic effect occur. Everybody assumes that Parkinson's is a disease of old age, but it is not clear to me on a genetic level. Part of the genetics of Parkinson's are correlated with the size of numerous brain regions, such as the striatum. And those measurements of brain size were taken mostly in people in their twenties. That suggests that there might be a developmental aspect to Parkinson's and if we want to know what we're going to drug, or when the process needs to be affected, we need to know whether it's developmental or late in life. We don't want to be attempting to drug a process in a 70-year old, that was actually active while they were a 4-month old embryo.”
Dr Skene believes we are only just getting started with exploiting the potential of these new methods and techniques.
“The single cell approaches are undergoing exponential change. It's impossible to even keep up with the methods as they’re developing so fast. When I first started, the largest single cell dataset had around 3000 cells. Now it's fairly routine to generate a dataset that has a million and we're looking at all kinds of different changes inside the cells.
I’m particularly interested in epigenetic changes, so changes that modify how DNA is used within a particular cell type. There is a new technology that I'm really excited about, which is single cell ‘cut and tag’, enabling us to study protein modifications around DNA. This is something we really need to be able to work on human tissue, but at the moment it's never been done using human nuclei. I'm excited to get this set up and working in the lab.”
Genetics and single-cell research have changed the game to such an extent that I think we can now solve the puzzle.Dr Nathan SkeneGroup Leader based at UK DRI at Imperial
With deeper understanding of the diseases that cause dementia, our appreciation of the vast complexity surrounding their origins also increases. But can this new knowledge translate into desperately needed treatments for dementia?
“First, we're going to need to identify which process within that cell is affected. I think it's going to be possible to do that. And it may turn out that the solution then is something as simple as a gene therapy target in that cell. I don't think we will need to be wildly specific, so targeting some particular gene. Any number of genes would probably do as long as you identify which process within that cell you need to inhibit or activate, but we have to do it through genetics. The genetics is fundamentally the only thing you know about these diseases.”
Another exciting branch of research that Dr Skene has become involved in is the Multi-‘omics brain atlas project (MAP), a £2M UK DRI initiative using an unprecedented range of advanced techniques to examine tissue from eight different regions of the Alzheimer’s brain to build understanding of the causes.
“The MAP project is essentially digitising the neuropathology of Alzheimer's disease. It is going to give us a whole new level of resolution of what actually goes wrong in the condition. My part of the project is to try to make the analysis as robust and open as possible. We want to make it so that everybody can access the data, everyone can replicate our analyses and build on them. I think that when it comes to large data-driven projects, the old-fashioned way of doing science, that you produce a PDF that remains the static representation of an analysis forever onwards, is just not really cutting it. There's no way to compress all the information that comes from a large -omics study into a single PDF. So, part of what we're trying to do with the MAP is to build a new approach to science and neuropathology. That will act as a resource for the whole community.”
Nathan has also been setting up his own collaborations to take his research further, drawing on expertise from pathologists, neuroanatomists and brain banks to collect data from several different regions of the human brain. With a background in Artificial Intelligence (AI) and Cybernetics, Dr Skene sees a huge benefit in machine learning, and is working closely with the recently established DEMON network – an initiative that facilitates the application of data science and artificial intelligence to dementia research. Although much of Nathan’s focus is on dementia, he suggests that the data produced has far greater potential and could help uncover the roots of other diseases.
“On my computer, I've got data on tens of thousands of human diseases where I can map them onto particular cell types, and I don't have time to publish everything that I've found. There are just not enough hours in the day. My lab’s goal isn’t to investigate whether gene therapy against a particular heart cell type works, for example. However, if there is a group that is interested in doing that then I'm happy to share the data with them and say, for example, ‘what you want to do is get a vector that's got a promoter.”

A brand new development at the heart of White City campus and home to UK DRI at Imperial
Having spent a year at the UK DRI, Nathan is optimistic about future therapies for dementia.
“I think throughout history there are certain problems that, when people have organised themselves, they've been able to achieve quite incredible things. People have proven again and again that they are capable of solving problems at an unimaginable rate. I think with the UK DRI, there's a possibility that we can do this for Alzheimer’s disease.
I view the disease as a genetic system with just another complex trait. But on another level, what that means is that if we solve Alzheimer’s, I think we can do the same for other conditions. The same basic approaches that will be necessary for learning how to tackle one complex disease will be required for all of them. It might open up lots of opportunities.
Genetics and single-cell research have changed the game to such an extent that I think we can now solve the puzzle. It will require that we bring together resources that are not currently there, but the basic steps for doing it are nearly in place. Biology itself needs to change. We need far more data scientists. We need more machine learning specialists. And we may need some new strategies. But I think the UK DRI probably has the best chance of doing this. Once we figure that out then solving it will be almost an engineering problem.”
For more information or to explore partnering opportunities, please contact UK DRI Director of Innovation and Business, Dr Kay Penicud.
Article published: 19 October 2020
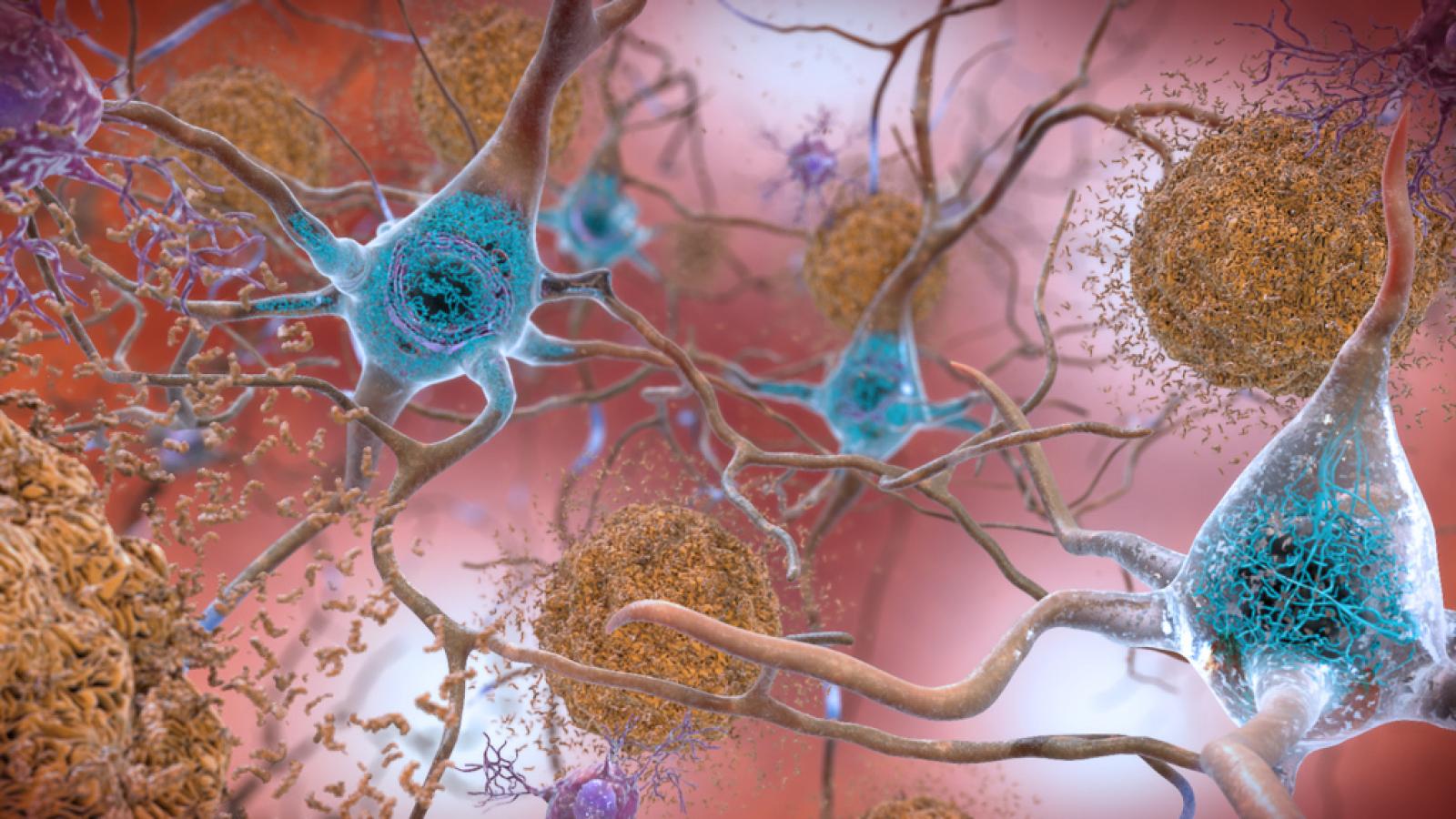
Banner image courtesy of National Institute on Aging, National Institutes of Health, U.S. Department of Health and Human Services.
Gene image: adike/Shutterstock.com