We’re thrilled to officially appoint our seventh centre of the UK DRI, after a competitive search for a robust programme that asks new and fundamental questions on how to better support people with dementia.
This ground-breaking £20m research centre will develop new technologies to create dementia-friendly ‘Healthy Homes’ and provide insights into how dementia develops.
<p>new centre</p>
Around 850,000 people in the UK have dementia, of which over 60 per cent are living in the community. Under the leadership of Prof David Sharp, this unique new centre will use a range of approaches - from artificial intelligence and robotics to sleep monitoring - to empower people with dementia to live safely and independently in their own homes.
Based at Imperial College London, in collaboration with the University of Surrey, the goal of the new centre is to develop technologies to enable people to live in their own homes for as long as possible, explains Professor David Sharp, Neurologist at Imperial College London and Associate Director of the new centre:
“The vision for this centre is to use patient-centred technology to help people affected by dementia to live better and for longer in their own homes. Latest figures suggest one in four hospital beds are occupied by people with dementia – and 20 per cent of these admissions are due to preventable causes such as falls, dehydration and infections. The new technologies we develop will improve our ability to support people in their homes. They will allow us to intervene at an early stage, to prevent the crises that so often lead to hospital stays, or a move to a care home. What’s more we’ll be able to improve our understanding of dementia onset and progression.”
The centre will be based at the Michael Uren Biomedical Engineering Research Hub, part of Imperial’s White City Campus. It will bring together scientists, engineers and doctors to build on existing, early-stage technologies that can be integrated into a person’s home. The idea is this technology continuously assesses physical and mental wellbeing, alerting a person’s medical team of any potential problems at an early stage.
<p>of people with dementia in the UK are living in the community</p>
Much of the current research activity in the UK DRI is basic neurobiology aimed at understanding the very earliest genetic, biochemical and cellular events that lead to dementia. We anticipate that a more complete understanding of these processes will enable us and others to design and test ways of preventing or slowing the disease process. The new UK DRI Care Research and Technology programme complements this ongoing work by taking a more patient-centric approach, which will make help make an impact in the shorter term.
<p>of the UK DRI work together</p>
Not only will the new programme result in exciting and novel technology to help patients live better lives in their own homes, but it will also deliver valuable data, direct from patients, that will provide insights into the underlying causes and progression of dementia. We warmly welcome Dave and his colleagues to the growing UK DRI family. His programme will be fully integrated into the Institute and, as our latest Associate Director, Dave will become part of the UK DRI leadership team.Prof Bart De Strooper and Dr Adrian IvinsonUK DRI Directors
Some of the technology developed at the centre will include:
- Sensors placed around the house or on a patient’s body to track vital signs such as heart rate, blood pressure and body temperature. The hope is these sensors – some of which are small enough to be worn as a small earpiece - will also provide key information such as gait, brain activity, and sleep that have previously been hard to measure in the home.
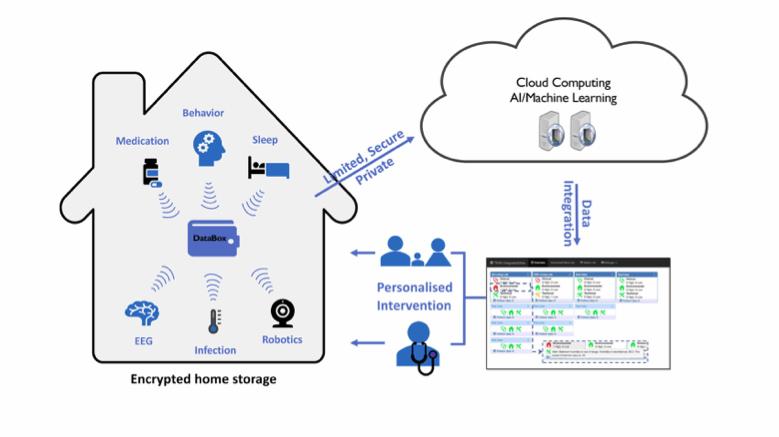
- Artificial intelligence that will automatically integrate all this patient information and flag any changes – for instance highlighting a change in walking pattern that might suggest a patient is at risk of a fall, or an elevated temperature that could suggest an infection.
- Technology that allows researchers and medical teams to that tracks a patient’s memory and cognitive function. The centre’s goal is to be able to monitor behaviour in the home with technology that doesn’t interfere with their everyday life - and then use this information to predict when patients might run into problems, such as if they begin to become agitated or distressed, and intervene early to assist them.
- Methods of tracking sleep quality. Sleep disturbance is a significant problem in dementia, but is hard to monitor at home. The centre will develop new ways to track sleep via motion sensors in the beds and bed sheets, and use this information to potentially improve sleep quality.
- Quick, simple at-home tests for common infections. Infections are a significant issue for people with dementia, and often lead to hospital stays. The centre will develop rapid tests that a carer can use, which send immediate results to their GP.
- Robotic devices that interact with patients living with dementia. These devices will assist by alerting patients to safety risks – such as spilt liquid on the floor or a cooker left on, in addition to monitoring if a patient seems agitated or distressed, and notifying the patient’s healthcare team.
<p>is at the heart of the research</p>
will use various sensors around the home and wearable devices to monitor sleep quality, behaviour, blood pressure, physical movement and brain activity. All this data
The new centre will collaborate closely with the University of Surrey. Professor Payam Barnaghi, Professor of Machine Intelligence at the University of Surrey, says “Stays in hospitals and care homes can be very distressing for people with dementia. Not only are they trying to navigate a new physical environment, they are distanced from their friends and families causing further distress. The technologies involved in this project will enable people to live independently at home whilst not sacrificing their care. Working with the latest machine learning capabilities means the technology we’re using will be able to get better at spotting warning signs and events that require intervention. Doctors will be able to have confidence in their ability to monitor people remotely and to react quickly to any worrying changes. Improving the quality of life of people with dementia is crucial to their and their families overall wellbeing.”

All of the technology developed at the new UK DRI Care Research & Technology centre will be assessed and evaluated by people living with dementia, and their carers, to ensure it is both practical and needed. Key to its success is people like Trevor.
Trevor Truman is a member of the new centre’s steering committee, and principal carer for his wife, who was diagnosed with Alzheimer’s disease in 2016. Trevor tested early prototypes of the technology that will be developed at the centre, as part of a trial, called Technology Integrated Health Management (TIHM), led by Surrey and Borders NHS Partnership NHS Foundation Trust and The University of Surrey.
Trevor explains:
“Most carers want to keep their loved one at home, safely, and feeling secure for as long as possible. Having experienced over twenty individual sensors or data-gathering devices in my home, I realise technology can play an important part in achieving this aim. Some sensors automatically monitor information such as sleep patterns, room temperature or unusual movements. Others, such as those that monitor blood pressure, weight, body temperature and hydration, require input from us.
This suite of technology allows the team to monitor my wife’s health and well-being remotely, and call the carer in any situation that creates concern. An example of this was when I received a call saying my wife may need to see her GP, based on her blood pressure readings from the technology. When we visited the GP, we were able to take my wife’s data with us – using the app on my tablet– giving our GP an instant overview of her health and recent history relevant to the visit. New medication was prescribed that day. It was quick, efficient, and effective for us, and can be for others too.
This monitoring service - that sees changing data, is alerted to changes, and can be in contact with clinicians 24/7, has made major steps forward in delivering a greater sense of security and confidence for patients during the project. It helps to release isolation, presents a human face for impersonal technology, and provides a measure of control over the incurable.
The matrix of health, capacity, emotions, anxieties, and uncertainties is constantly varying with every dementia patient. The clear need, and the aim of this project, is for a new, adaptive system. One that will integrate the best and most suitable technology, data collection, and analysis - and apply it appropriately and effectively to each individual patient’s changing condition.
At the heart of this approach is the goal of using technology to help people provide the best possible care for their loved one on their journey through dementia - keeping them safe and secure at home for longer."
<p>will assess and evaluate the new technology</p>
Advanced technologies such as robotics and Artificial Intelligence have great potential to support us in illness or old age. This project will help those living with dementia stay in their own homes for longer, with the dignity and independence we all deserve. One of our modern Industrial Strategy’s Grand Challenges is Ageing Society, and that is why we are backing new research like this to help us all adapt to our society where people come first.Chris SkidmoreScience Minister
Scientists at the centre have already developed safe and robust data storage technologies, to ensure all personal data is secure.
Following formal processes, the new centre will open on 1 June 2019.
