A new study led by Prof David Sharp, Centre Director at UK DRI Care Research & Technology, has used a state-of-the-art blood test to track damage to the brain in people who have sustained traumatic brain injury (TBI). Measuring the protein biomarker in the blood will provide a simpler, more accurate way to predict clinical outcomes and may help to identify those at higher risk of developing dementia. The study is published today (29 September) in Science Translational Medicine.
Around 50 million people each year worldwide experience TBI as a result of head injury. In the brains of these individuals, the neurons encounter severe stretching and sheering forces which cause damage to their axons, the part which transmits electrical signals. Axonal damage is the best predictor of clinical outcomes and recovery but has been difficult to measure in patients.
The team from the UK DRI Care Research and Technology Centre, based at Imperial College London, set out to identify a chemical that could be easily detected in the blood - a biomarker - that would accurately reflect this axonal damage in the brain after TBI. A multicentre study was established involving over 200 patients who had experienced moderate to severe TBI, recruited from eight major trauma centres across Europe. In 56% of cases the injuries were classed as ‘high energy’, involving falls from over 3 metres or collisions at more than 30km/hour, with the majority of these caused by road traffic accidents.
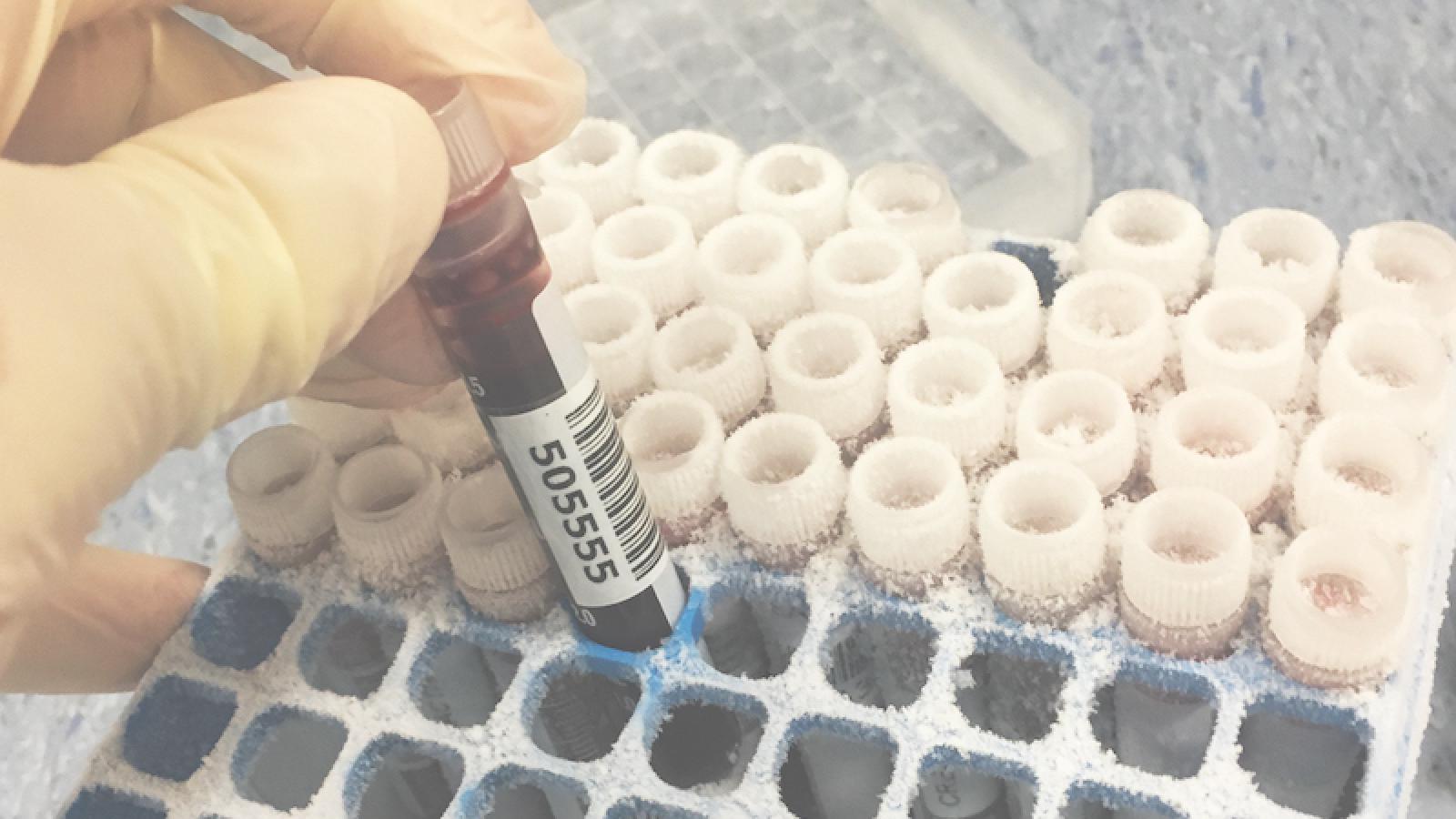
To find a suitable protein marker, the researchers harnessed cutting-edge technology called single molecule array (SiMoA) that can measure sub-femtomolar (10-16) levels of chemicals in the blood. Starting their search by detecting proteins that are important to the structure of the axons, they found that measuring blood levels of neurofilament light provided a remarkably accurate long-term prognosis for the patient. Neurofilament light has become a useful tool for diagnosis, monitoring and prognosis across neurodegenerative disease like Alzheimer’s, but its potential for use in TBI has not been fully assessed and optimised until now.
people each year worldwide experience TBI as a result of head injury
If we could roll the neurofilament light test out across the country, it would be hugely impactful. We’re gearing up to offer it to NHS patients at Imperial in the near future.Dr Neil Grahamjoint first author and ARUK Clinical Research Fellow based at the UK DRI’s Care Research and Technology Centre
Dr Neil Graham, joint first author and Alzheimer’s Research UK Clinical Research Fellow based at the UK DRI’s Care Research and Technology Centre, based at Imperial College London, said:
“I’m extremely excited by the ultrasensitive blood test technology we used here as it has opened up a whole new world of possibilities when it comes to precise injury diagnosis and prediction of outcomes after head injury. This is particularly useful in the area of dementia risk assessment after TBI, which is very challenging at present. If we could roll the neurofilament light test out across the country, it would be hugely impactful. We’re gearing up to offer it to NHS patients at Imperial in the near future.”
The team also used advanced types of brain imaging to validate blood test findings. Blood levels of neurofilament light were found to be closely related to measures from diffusion MRI, an advanced type of imaging which also provides measures related to damage to axons. The team also compared blood levels of neurofilament light with a special type of brain imaging that measures shrinkage (atrophy) of the brain, indicating the loss of nerve cells. They found that blood levels of neurofilament light tracked extremely well to brain atrophy and importantly predicted further nerve cell degeneration up to one year after the injury. These findings mean future blood tests could provide similar information to MRIs, but in a more cost-effective and accessible manner.

MRI brain scans from patients in the TBI study
Dr Karl Zimmerman, joint first author and postdoctoral researcher based at the UK DRI’s Care Research and Technology Centre, based at Imperial College London, said:
“These results are exciting as they pave the way for the use of these advanced biomarkers in the assessment of head injuries in other contexts. We have studied and shown that there may be similar changes occurring in professional athletes exposed to head injuries. We’re setting up more research to look at this in detail to improve care of sportspeople concerned with later life risk of dementia.”
In order to further validate the blood biomarker findings, the team also analysed fluid samples from around the damaged neuronal axons. Following surgery in some of the patients, such as a craniotomy to remove part of the skull, the team inserted catheters into the brain. With simultaneous measurements taken from the blood, the researchers were able to identify a strong correlation, supporting evidence that the protein in the blood originated at the source of the damage, and so reflected well the progressive damage taking place in the brain.
Prof David Sharp, senior author of the paper and Director of the UK DRI’s Care Research and Technology Centre based at Imperial College London, said:
“Outcomes after TBI are very difficult to predict. This is a major challenge for doctors trying to care for patients recovering from head injuries of all severities. What we need are more accurate diagnostic tests that can be used in our major trauma units and clinics. Our work shows that measuring neurofilament light soon after head injury helps predict who will develop long-term problems. We are applying this in various contexts, including for the investigation of sporting TBI, and will be investigating whether this blood test can be used to predict those at high risk of developing dementia”
Dr Rosa Sancho, Head of Research at Alzheimer’s Research UK, said:
“Traumatic brain injury is a risk factor for dementia, and identifying the long-term impact of individual head injuries remains an important goal for research. This work gets us closer to a blood test able to predict how brain changes develop up to one year after injury. Dementia develops over many years and we need to build on these findings to help improve longer-term prognosis and to reliably determine an individual’s risk of dementia following a head injury.
As the UK’s leading dementia research charity, we’re pleased to have funded both Dr Graham’s clinical work and the UK DRI. We couldn’t do either without the continued dedication of our supporters.”
Reference
Neil S. N. Graham, Karl A. Zimmerman, Federico Moro, Amanda Heslegrave, Samia Abed Maillard, Adriano Bernini, John-Paul Miroz, Cornelius K. Donat, Maria Yanez Lopez, Niall Bourke, Amy E. Jolly, Emma-Jane Mallas, Eyal Soreq, Mark H. Wilson, Gavin Fatania, Dylan Roi, Maneesh C. Patel, Elena Garbero, Giovanni Nattino, Camelia Baciu, Enrico Fainardi, Arturo Chieregato, Primoz Gradisek, Sandra Magnoni, Mauro Oddo, Henrik Zetterberg, Guido Bertolini, David J. Sharp (2021) Axonal marker neurofilament light predicts long-term outcomes and progressive neurodegeneration after traumatic brain injury Science Translational Medicine. Vol 13, Issue 613. DOI: 10.1126/scitranslmed.abg9922
Article published: 29 September 2021
Images courtesy of Dr Neil Graham and Karl Zimmerman