In a new mouse study, scientists led by Prof David Rubinsztein (UK DRI at Cambridge) have revealed that a repurposed HIV drug can restore the brain’s ability to clear out toxic proteins, which is impaired in Huntington’s disease and other forms of dementia. The research, published in the journal Neuron, offers clues to how the build-up of toxic proteins could in future be slowed or prevented in humans.
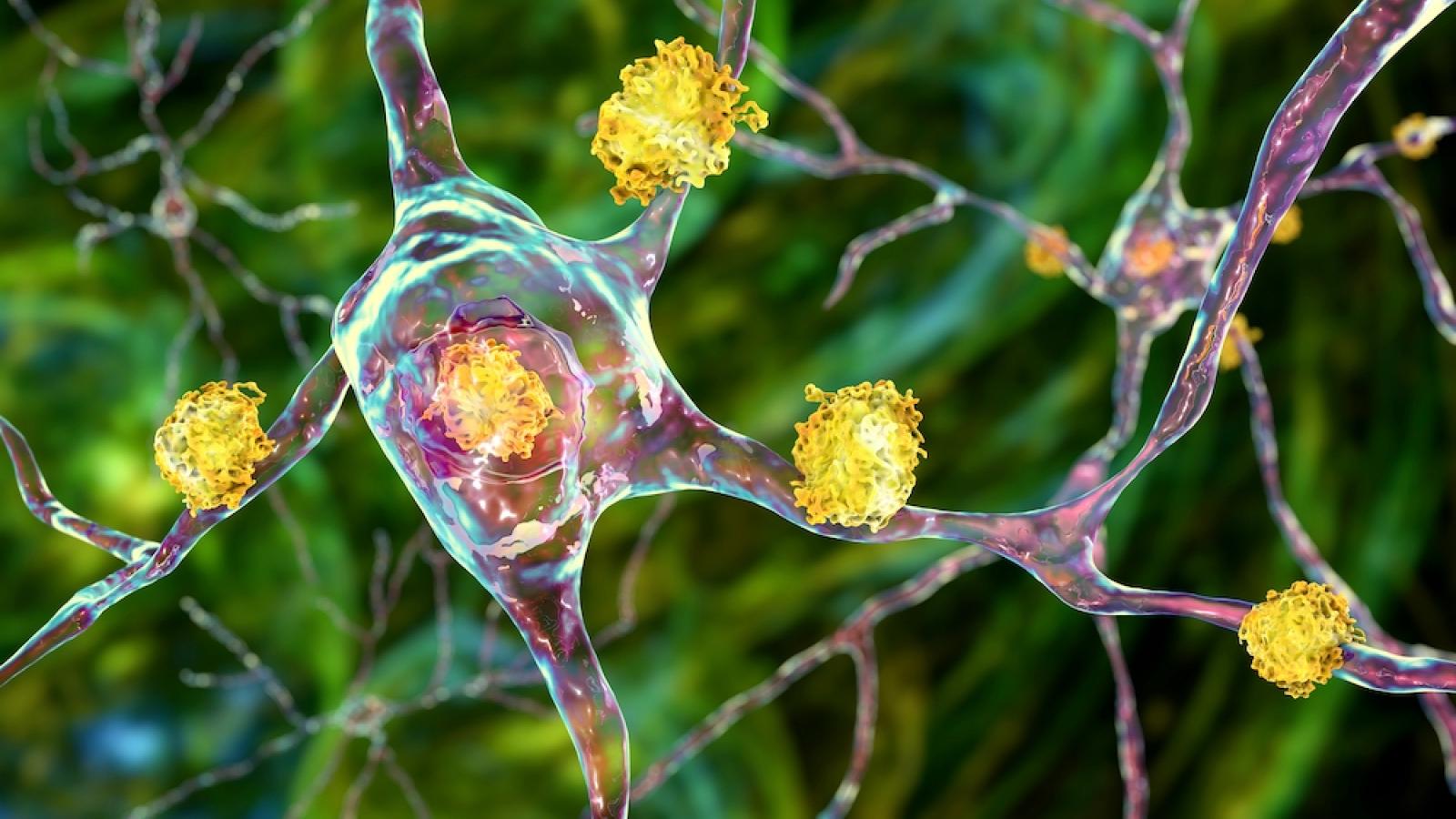
A common characteristic of neurodegenerative diseases such as Huntington’s is the build-up in the brain of clusters – known as aggregates – of misfolded proteins, such as huntingtin and tau. These aggregates are thought to lead to the degradation and eventual death of brain cells and the onset of symptoms.
One method that cells in our body use to rid themselves of toxic materials is autophagy, or ‘self-eating’, a process whereby the cells ‘eat’ the unwanted material, break it down and discard it. But there is evidence autophagy is disrupted in neurodegenerative diseases, meaning that the cells are no longer able to remove the harmful misfolded proteins.
is activated in neurodegenerative disease and impairs the brain's ability to rid itself of toxic proteins
We’re very excited about these findings because we’ve not just found a new mechanism of how our microglia hasten neurodegeneration, we’ve also shown this can be interrupted, potentially even with an existing, safe treatment.Prof David RubinszteinInterim Centre Director at the UK DRI at Cambridge
In this study, the team from the UK DRI at Cambridge and the Cambridge Institute for Medical Research identified a process that causes autophagy to become dysfunctional in the brains of two different mouse models, a model of Huntington’s and a model of tauopathy – and importantly, a drug that helps restore this vital function.
The brain’s resident immune cells, known as microglia, should protect it against unwanted and toxic materials. In neurodegenerative diseases, the microglia kick into action, but in such a way as to impair autophagy.
In mice, the team showed that in neurodegenerative disease, microglia release a suite of molecules which activate a switch on the surface of cells. When activated, this switch – called CCR5 – impairs autophagy, and hence the ability of the brain to rid itself of the toxic proteins. These proteins then aggregate and begin to cause irreversible damage to the brain.
Prof Rubinsztein explained:
“The microglia begin releasing these chemicals long before any physical signs of the disease are apparent. This suggests – much as we expected – that if we’re going to find effective treatments for diseases such as Huntington’s, these treatments will need to be given before an individual begins showing symptoms.”
When the researchers used mice bred to ‘knock out’ the action of CCR5, they found that these mice were protected against the build-up of misfolded huntingtin and tau. This discovery indicates how the build-up could in future be slowed or prevented in humans. Interestingly, the CCR5 switch is not just exploited by neurodegenerative diseases – it is also used by HIV as a ‘doorway’ into our cells.
The team used a drug called maraviroc, approved for treatment of HIV, to treat the mice, administering the drug for four weeks when they were two months old. When the researchers looked at the brains of the mice, they found a significant reduction in the number of aggregates when compared to untreated mice. In the tauopathy model, the drug was also found to slow down memory loss.
Prof Rubinsztein added:
“We’re very excited about these findings because we’ve not just found a new mechanism of how our microglia hasten neurodegeneration, we’ve also shown this can be interrupted, potentially even with an existing, safe treatment.
Maraviroc may not itself turn out to be the magic bullet, but it shows a possible way forward. During the development of this drug as a HIV treatment, there were a number of other candidates that failed along the way because they were not effective against HIV. We may find that one of these works effectively in humans to prevent neurodegenerative diseases.”
To find out more about Prof David Rubinsztein’s research, visit his UK DRI profile. To stay up to date on the latest UK DRI news and events, sign up to receive our monthly newsletter, ‘Inside Eye on UK DRI’.
Reference: Festa, BP, Siddiqi, FH, & Jimenez-Sanchez, M, et al. Microglial-to-neuronal CCR5 signalling regulates autophagy in neurodegeneration. Neuron; 26 Apr 2023; DOI: 10/1016/j.neuron.2023.04.006
Article published: 26 April 2023
Banner image: Shutterstock/Kateryna Kon