A new study led by Dr Barry McColl and Dr Jack Barrington (UK DRI at Edinburgh) reveals insight into cellular changes in the brain that occur after a stroke. The research, published in the journal Cell Reports, could open up new therapeutic avenues for the condition.
What was the challenge?
People who have had a stroke often experience disability and cognitive impairment, and stroke contributes the greatest global disease burden of all neurological conditions.
Acute ischaemic stroke, where a blockage (plaque or blood clot) cuts off the blood supply to part of the brain, triggers an inflammatory reaction. Macrophages and monocytes, types of white blood cell, accumulate around the damaged tissue.
However, there is growing recognition that this type of injury also triggers structural and functional changes throughout the brain, including in remote areas connected by fibres of white matter to the site of the stroke. The chronic physical and cognitive symptoms experienced by people who have had a stroke may result from altered brain function caused by these brain-wide changes. In this study, the team set out to investigate changes in the brain that occur after a stroke, and how different cell types respond to the damage.
These insights will help us develop new therapeutic strategies aimed at modifying immune responses to enhance recovery and cognitive function in people affected by stroke.Dr Barry McCollUK DRI at Edinburgh
What did the team do and what did they find?
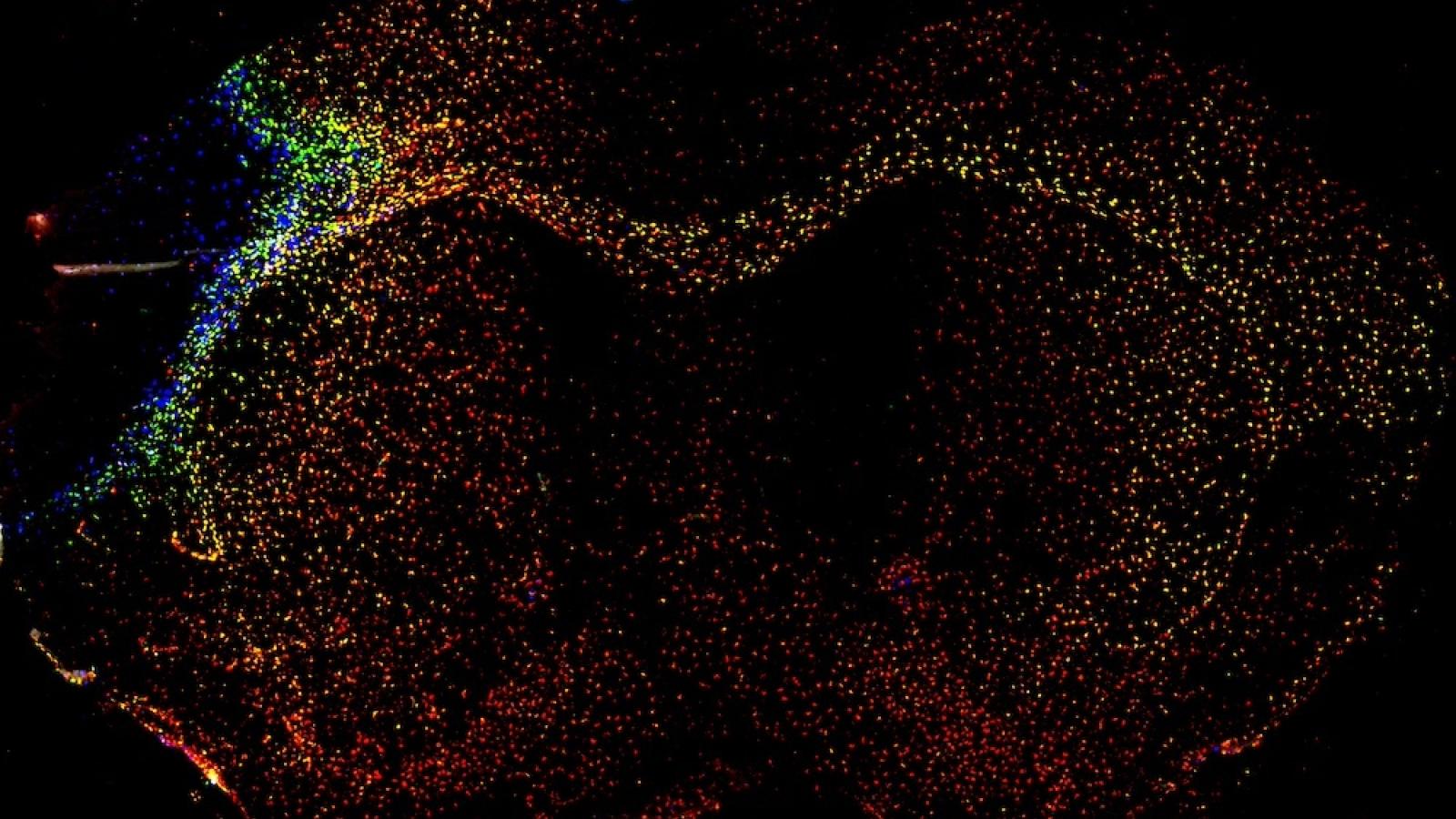
Through studying macrophages in a model of stroke, the researchers discovered that stroke increases the variety of immune cells in specific patterns. Near the stroke-damaged area, different types of immune cells (some originally from the brain and some from the blood) mix together. Some of these cells take on roles related to handling fats and repairing tissue.
In areas farther from the stroke but connected by white matter fibres, only microglia – the brain’s resident immune cells – become active, without help from other immune cells. The remote activation of microglia involves production of chemokines, a type of signalling protein, which are important for cell communication. The team also found a link between cell division and certain active states of microglia, which might help to explain how these active states develop.
What is the impact of these findings?
These findings suggest that the brain's immune response to a stroke is widespread but organised based on brain structure. The response might affect overall brain health, its ability to adapt, and how different parts of the brain communicate. Future research will use new techniques to track microglia from the time they become active and those involved in chemokine signalling over a long period. This research could reveal how these cells develop, their long-term roles, their impact on brain function, and identify new ways to modify immune responses in the brain.
Dr McColl explained:
"Our study sheds light on under-recognised aspects of the immune response in the brain post-stroke, revealing organised patterns of immune cell activity that extend beyond the immediate injury site. These insights will help us develop new therapeutic strategies aimed at modifying immune responses to enhance recovery and cognitive function in people affected by stroke."
Dr Barrington added:
“Our work really emphasises the power of combining single-cell and spatial profiling approaches to uncover important features of brain biology. These tools have facilitated our understanding of the key players in the brain-wide response to stroke and their relationship with spatially distinct pathophysiological processes.
The knowledge gained from this study has inspired new research directions that we think will be important in identifying the cellular/molecular targets of future disease-modifying treatments.”
To find out more about Dr Barry McColl's research, visit his UK DRI profile. To keep up to date with the latest UK DRI news and events, sign up to receive our monthly newsletter.
Article published: 6 June 2024
Banner image: McColl lab