In September, it was announced that anti-amyloid treatment lecanemab had been successful in slowing cognitive decline in people with mild cognitive impairment and early Alzheimer’s. The first of its kind to show clinical benefit, and potentially disease modifying capabilities, the development has been labelled a breakthrough, and even hailed as the ‘beginning of the end’ for life-changing therapies for the condition.
Following presentation of the Phase III data at the Clinical Trials on Alzheimer's Disease conference (CTAD) in November, together with a publication in the New England Journal of Medicine, the UK DRI hosted a roundtable to dig into the data and what it means for the future of Alzheimer’s treatments and clinical translation.
The panel consisted of experts whose specialties stretched across the pipeline from fundamental scientific discovery, through drug translation and into clinical practice. Further details on the panel can be found below along with a public recording of the event.
Clinician Prof Jonathan Schott chaired the session, together with UK DRI Director of Scientific Affairs Dr Giovanna Lalli, summarising the main results from the Clarity AD Phase III trial, and introducing the purpose of the roundtable as a platform to pave the way for discussions we need to be having in the future.
Dr Catherine Mummery provided a historical overview on amyloid treatments to date, and how the Clarity AD trial differed in design, enrolling participants at earlier stages of disease, lower amyloid burden and from a more ethnically diverse pool. The encouraging data demonstrated a reduction in CSF and blood biomarkers, and consistent positive results across a range of clinical outcomes including both cognitive measures and those related to activities of daily living and carer burden.
Focusing on the underlying biological mechanisms, UK DRI Director Prof Bart De Strooper discussed his recent work with Dr Eric Karran, describing how it appears that amyloid load needs to be cleared to certain threshold, and maintained, in order to see clinical benefit. Although lecanemab has been shown to reduce amyloid burden the quickest, it could be speculated that benefits would be also observed with longer amyloid trial designs, or other related targets like the gamma-secretases.
Prof James Rowe led attendees through the opportunities and challenges that lecanemab poses for translational research, additionally highlighting where this drug sits in the context of other ongoing clinical trials. It’s notable that many of the disease-modifying treatments target the other hallmarks Alzheimer’s, including inflammation, Tau and synapse loss. Prof Rowe urged consideration of the complex pathophysiology of this disease, which is still not fully understood, and the likely need for multiple different treatments and combinations in future.
Prof Clare Mackay finished the panel presentations by reviewing the infrastructure and mechanisms that need to be in place to deliver treatments to people living with Alzheimer’s in the UK. A significant challenge lecanemab poses is the complex protocol requiring amyloid positive diagnosis, IV administration of the drug every two weeks and regular MRI scans to ensure safety – something the healthcare system is currently not able to roll out. Prof Mackay presented a recent pilot of the Brain Health Clinic Network as a novel pathway for patients to receive a diagnosis, while also collecting valuable data to feed into future research.
An engaging Q&A followed the panel presentations where recurring topics included:
- Why it appears men responded more positively to lecanemab in the trial
- What the biomarker data from the trial showed and future innovations in this area
- What the long term effects of the drug might be and whether patients will require treatment for the rest of their lives
- What the best time for intervention is and who should receive the drug
- What the risks associated with the treatment are, and can ARIA be overcome with antibody therapies
- What would be considered a meaningful clinical effect for the patient
We’d like to again thank the panelists and attendees for their participation in this fascinating roundtable discussion. If you would like to stay updated on future events from the UK DRI, please sign up to our monthly newsletter.
Article published: 04 January 2023
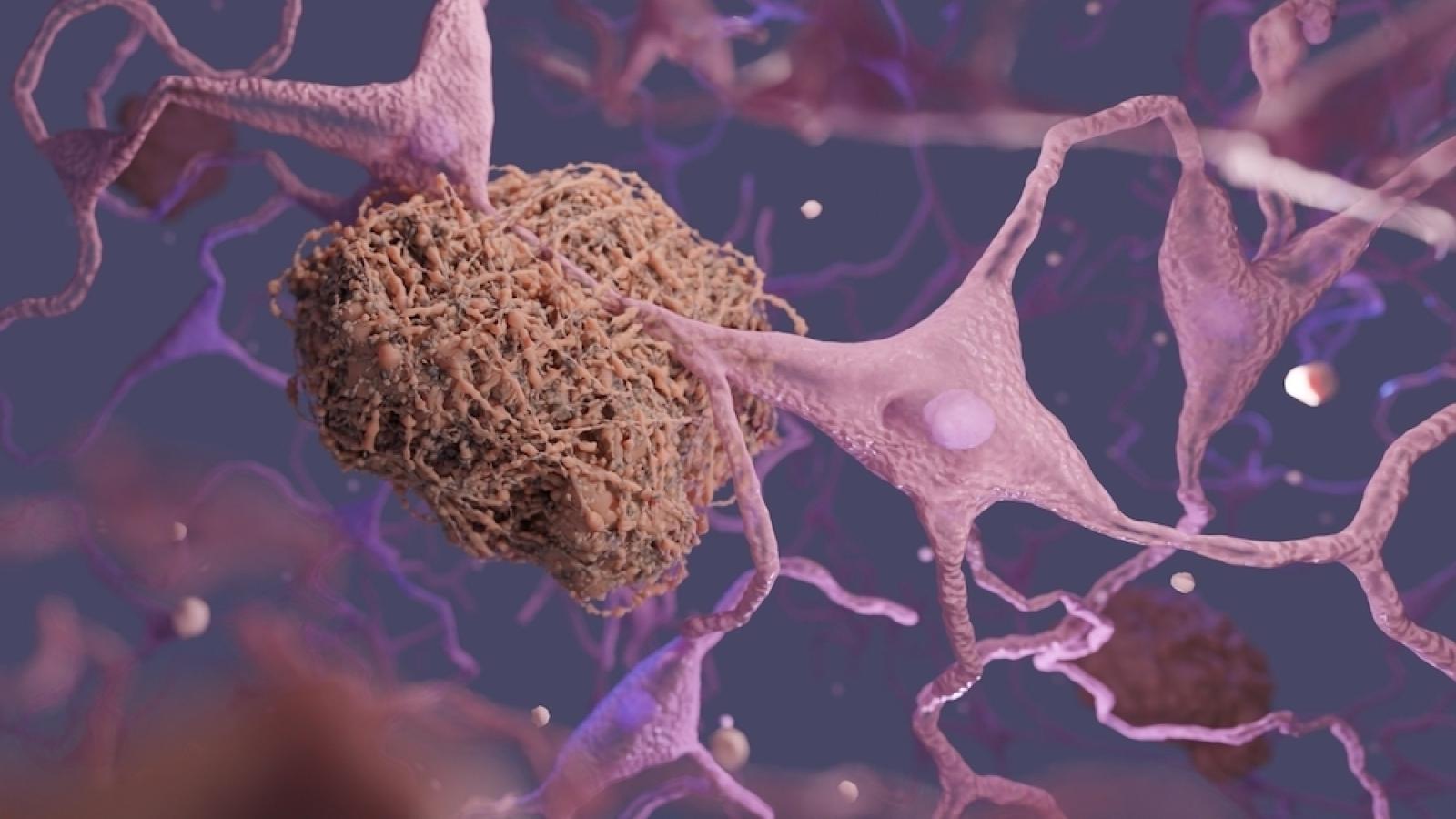
Banner image: Shutterstock / Signal Scientific Visuals