What is Alzheimer’s disease?
Alzheimer’s disease is a ‘progressive neurological condition’, which means that it affects the brain, and symptoms get worse over time. It impacts memory and other aspects of thinking, eventually impairing people’s ability to carry out everyday tasks.
The condition starts gradually, with early symptoms – such as forgetfulness – often mistaken for a normal part of ageing. As Alzheimer’s progresses, it can significantly impact communication, decision-making, and independence.

Frequently asked questions
- How common is Alzheimer's?
Alzheimer’s is the most common form of dementia, making up 60-80% of one million dementia cases in the UK1.
Alzheimer’s becomes more common with age. It affects around 1 in 14 people over the age of 65 and 1 in 6 people over the age of 802. It’s predicted that the number of people with Alzheimer's in the UK will grow to 1.4 million by 2040, as our population gets older1. While it mostly affects older adults, people under 65 can experience early- or younger-onset Alzheimer’s.
- What are the symptoms of Alzheimer's?
Alzheimer’s has several stages, each with different symptoms:
- Early stage: Early symptoms are often subtle and may be mistaken for the normal signs of ageing. Symptoms most commonly include lapses in memory, such as forgetting recent events, names or where things are kept. People may also find themselves getting lost, struggling to remember the directions to familiar places, becoming increasingly disorganised and having difficulty with more complex tasks that involve planning and multi-tasking. They can also experience mood changes such as anxiety or irritability. Particularly in the early stages, these problems may go unnoticed by the person affected by them and are often first identified by their relatives or friends.
- Middle stage: Memory issues become more severe, making recognising family and friends or following conversations difficult. Other aspects of thinking become increasingly affected, including worsening planning and judgement, difficulty finding words, and difficulty with numbers. Managing daily tasks such as handling money or cooking becomes challenging. Wandering (particularly at night) and sleep disturbances are also common.
- Late stage: Eventually, many people living with Alzheimer’s will need full-time care. At this stage, symptoms can include more severe memory loss, personality changes and difficulty eating, dressing and bathing. People may find communication very difficult and become less mobile.
While, in the majority of Alzheimer’s cases, the earliest problems relate to difficulties with memory, in a small minority of people Alzheimer’s can present with different initial symptoms, including prominent problems with visual processing (known as posterior cortical atrophy) or with language (known as logopenic variant primary progressive aphasia). In these rarer atypical forms of Alzheimer’s disease, symptoms often develop earlier, in the 50s or early 60s.
There's more information about symptoms on the Alzheimer’s Society and NHS websites.
- How is Alzheimer's diagnosed?
As with many health conditions, individual experiences of Alzheimer’s can look different from person to person. If you or someone you care about is experiencing symptoms, please contact your GP for an initial assessment.
If the GP thinks the symptoms may indicate a form of dementia, they will refer the individual for a specialist assessment.
There’s currently no single test for Alzheimer’s. The specialist will look at a range of different things by:
- Reviewing the individual’s medical history, including how their symptoms have developed and the impact these symptoms are having on their life
- Completing a physical examination and testing different aspects of the person’s memory and thinking
- Ordering blood tests to rule out other conditions
- Arranging a brain scan to look for patterns suggestive of possible Alzheimer’s disease as well as excluding some of the other potential causes
- In some cases, using more advanced testing including a lumbar puncture (to examine the spinal fluid) or an advanced type of brain scan called PET
If an individual receives an Alzheimer’s diagnosis they will have the opportunity to talk through the next steps and understand what support is available.
If you or someone you know has been diagnosed with Alzheimer’s, you can find more information and resources on the Alzheimer’s Society’s website.
- What treatments are there for Alzheimer’s?
Research into Alzheimer’s has recently led to promising new medicines which it is hoped will help to slow or stop the condition from progressing. There are also non-medical treatments which can help individuals and their families manage symptoms and improve their quality of life. As of summer 2024, these include:
- Medications: Approved medications in the UK include cholinesterase inhibitors (donepezil, rivastigmine, galantamine) and memantine. These drugs can help to improve some of the thinking or memory symptoms people experience, but they do not slow or stop the underlying process that is damaging the brain and therefore unfortunately do not affect the long-term outlook. Two new treatments – Lecanemab (Leqembi) and donanemab (Kisunla) - have both been shown to alter the underlying brain changes and slow down the gradual impact that Alzheimer’s has on a person’s memory. Lecanemab is approved for use in the UK but is not available on the NHS.
- Psychological therapies: Approaches such as cognitive stimulation therapy (CST), cognitive rehabilitation and reminiscence therapy can help to support memory and cognitive function without medication. These treatments are designed to improve thinking, communication and overall wellbeing.
- Lifestyle interventions: A healthy lifestyle can help people manage the symptoms of Alzheimer’s. Staying active, socialising and doing mental exercises such as puzzles can all help to keep people’s minds active and improve their overall health.
More information on the different treatment options for Alzheimer’s can be found on the NHS or Alzheimer's Research UK websites.
- How can I get involved in research and trials for Alzheimer's disease?
If you’d like to get involved, Join Dementia Research is a great place to start. It’s a national service that connects volunteers with researchers who are looking for people to take part in their studies and includes opportunities for both people living with dementia and healthy individuals to contribute to research. By signing up, you can be matched to studies based on your health, location and other criteria, making it easier to find suitable opportunities.
- What support is available for Alzheimer's?
Support is crucial, not only for those living with Alzheimer’s but also for their families and carers.
For more information about support available, visit our page on ‘support for people affected by dementia’.
What causes Alzheimer's disease?
We don’t yet know exactly what causes Alzheimer’s, but research suggests it’s likely to be a mixture of factors, including genetics, lifestyle and the environment.
Age is the biggest risk factor for the condition with the late-onset, sporadic (i.e., not genetically caused) form being by far the most common. In rarer cases, known as early- or young-onset Alzheimer’s, symptoms can begin before the age of 50.
In the vast majority of cases, Alzheimer’s disease is not genetically inherited. However, in a very small proportion (less than 1% of cases) the condition is caused by a single genetic abnormality. This is known as familial Alzheimer’s disease, with affected individuals usually developing symptoms at a much younger age.
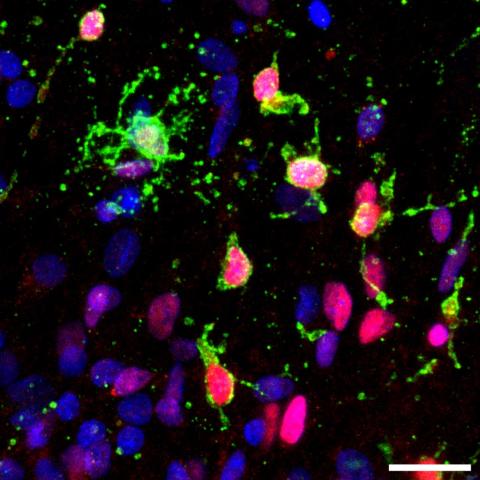
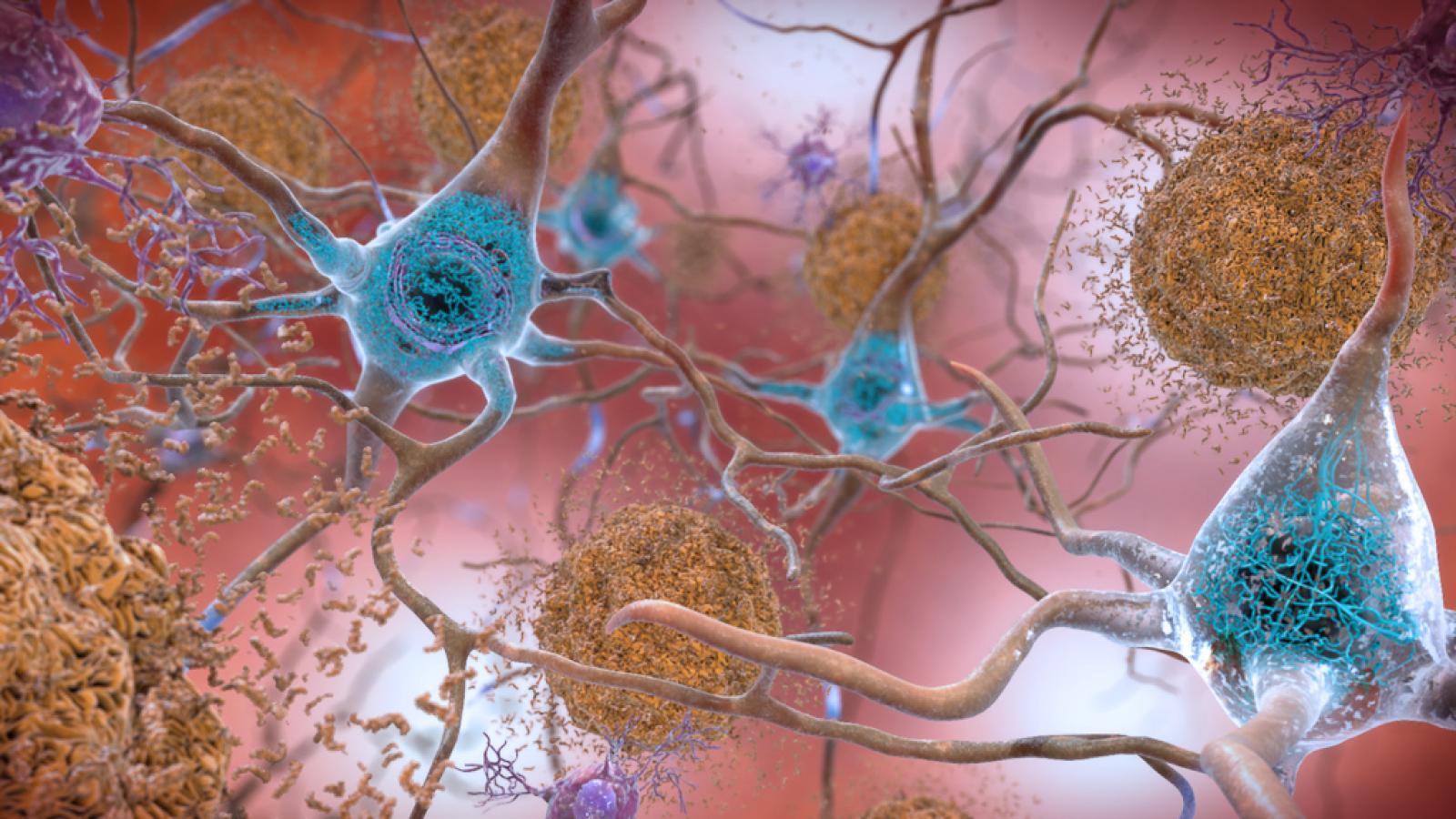
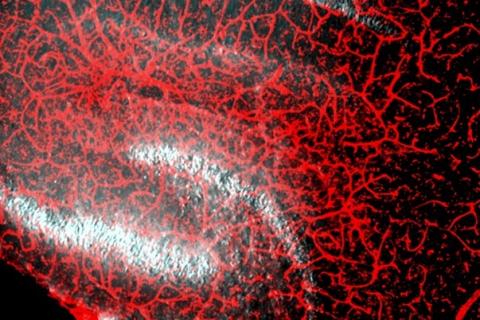
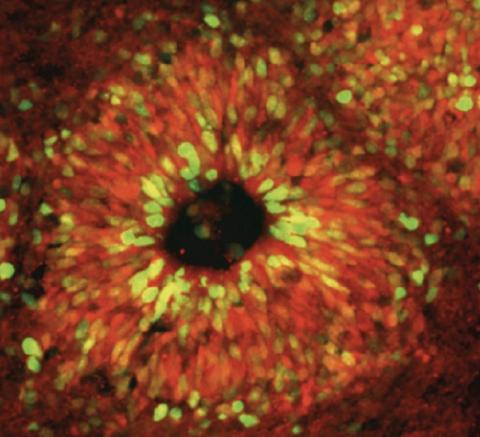
In the Alzheimer’s brain, there is a build-up of abnormal proteins in and around the cells, known as amyloid beta and tau. These stick together to form structures known as amyloid beta plaques and tau neurofibrillary tangles. These structures are linked to poor functioning, and the eventual loss, of neurons, which leads to the gradually worsening symptoms of the condition.
There are still many gaps in our understanding of the main causes of Alzheimer’s. Filling in these gaps could unlock new treatment options. Our researchers are at the forefront of existing and emerging theories, making discoveries to unlock the causes of Alzheimer’s and, crucially, develop interventions to stop it in its tracks.
Finding people during the early stages of Alzheimer’s, before the brain has been significantly damaged, will give us the best chance of developing effective treatments. At the UK DRI, we have the world’s leading facility dedicated to developing an accurate blood test for Alzheimer’s - the UK DRI Biomarker Factory. We have also invested in two other multi-million-pound projects to find new ways of diagnosing the condition.
The first drugs shown to slow down the disease, lecanemab and donanemab, both target the protein amyloid beta. The discoveries that led to these treatments were made decades ago by researchers including UK DRI Group Leader Prof Sir John Hardy. He proved that changes in the amyloid beta gene were directly linked to a genetic form of Alzheimer’s.
Other promising areas of research include:
- How other cells in the brain interact with neurons to either support or cause further harm.
- The role of our immune system, particularly the way that specialist immune cells in the brain react to amyloid beta and tau proteins.
- How proteins in the brain are processed and become abnormal/misfolded.
- How abnormal proteins cause connections between neurons (synapses) to break down.
- How our genetic makeup determines risk and can provide clues to the main causes of Alzheimer’s.
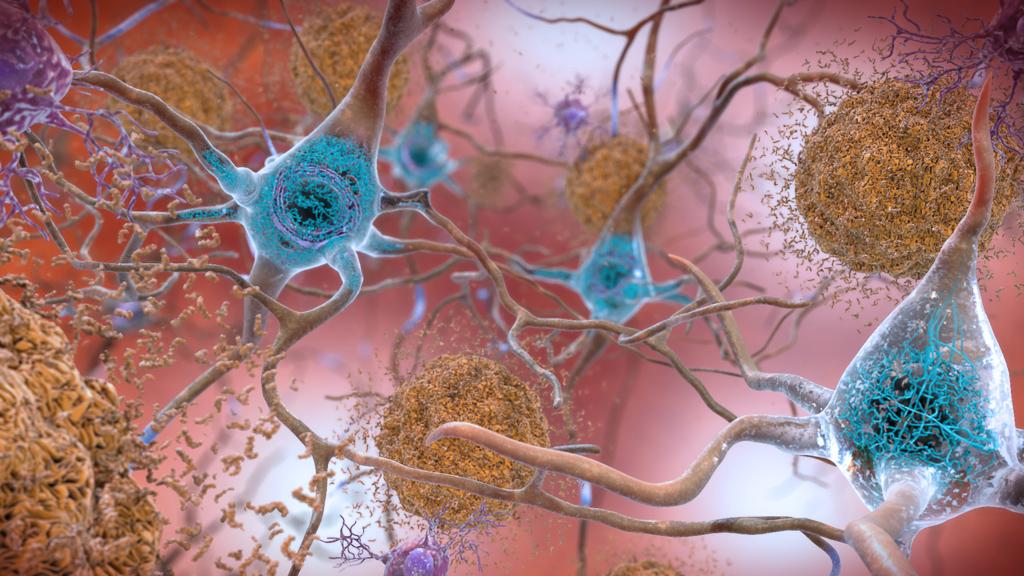
The main pathological protein hallmarks of Alzheimer's - amyloid beta plaques and tau neurofibrillary tangles. Credit: NIH.
Latest news