Having established a foundation of outstanding discovery science in its first five years, the UK DRI is set to capitalise on new insights into the causes and drivers of neurodegenerative disease with a programme of funding awards targeted at the translation of knowledge into urgently-needed treatments, technologies and diagnostics for dementia.
In the latest round of UK DRI translational awards, seven projects have been awarded funding in the region of £175-300k, representing a £1.7m investment from the Institute. They range from biomarker diagnostics and innovative monitoring technology, to promising disease-modifying treatments targeting mechanisms such as protein degradation and neuroinflammation.
UK DRI Director, Prof Siddharthan Chandran said:
“It’s wonderful to the see the UK DRI’s investment in discovery science bearing fruit, with the knowledge acquired from these studies showing therapeutic potential. It’s essential that we pursue and back promising avenues of investigation, so that we can change the outcomes for people with or at risk of developing dementia.
Neurodegenerative diseases are a complex set of disorders and I am particularly pleased with the diversity of approach taken in the successful projects, reflecting the ingenuity of our researchers across the Institute. A large number of the submissions also include close collaborations with Alzheimer’s Research UK’s Drug Discovery Alliance, showing the strength of the UK’s dementia research infrastructure and ecosystem.”
Dr Frances Wiseman and Prof Paul Morgan are two of the successful projects awarded funding, respectively aiming to identify a new diagnostic biomarker and develop a disease-modifying treatment for Alzheimer’s.
Developing and validating a new biomarker for Alzheimer's in high-risk populations
Dr Frances Wiseman (UK DRI at UCL), Dr Natalie Ryan (UK DRI at UCL), Prof Andre Strydom (KCL) and Prof Marie-Claude Potier (ICM)
The recent successes of lecanemab and donanemab in targeting the removal of amyloid beta protein from the brains of people living with Alzheimer’s, has revitalised the field of neurodegeneration and provided hope for millions affected worldwide. People with a genetic predisposition to Alzheimer’s, such as those with autosomal dominant familial Alzheimer’s (ADAD) or Down syndrome (DSAD), stand to gain most from these developments as they can be identified early in disease progression and treatment initiated when it is likely to have most effect.
Dr Frances Wiseman and colleagues are passionate to ensure that people living with these rarer forms of Alzheimer’s are considered in upcoming treatment opportunities and believes their inclusion could provide wider scientific insight and benefit for all people affected by the condition. However, side effects such microbleeds and swelling of the brain (ARIA (Amyloid Related Imaging Abnormalities)), can pose a significant risk to some individuals, especially for people with ADAD and DSAD who show build-up of amyloid within the brain’s blood vessels (cerebral amyloid angiopathy (CAA)).
Currently there is no way of identifying individuals with high CAA load, and therefore those at highest risk of side effects from amyloid-targeting therapies. This multi-disciplinary collaborative team aims to develop novel blood and imaging biomarkers to address this, helping clinicians make informed decisions on whether an individual should receive this type of treatment for Alzheimer’s.
Targeting neuroinflammation as a treatment for Alzheimer's disease
Prof Paul Morgan (UK DRI at Cardiff), Dr Wioleta Zelek (UK DRI at Cardiff) and Dr Emma Mead (Oxford Dementia Drug Discovery Institute)
Complement is part of our innate immune system, and a potent driver of inflammation in defence against pathogens. The over-activation of complement, however, is deleterious and contributes to many inflammatory diseases, with several successful anti-complement therapies now used in the clinic. It is thought over-activation of complement may play a key role in the progression of Alzheimer’s disease but current anti-complement treatments are not able to gain access to the brain.
Building on a previous UK DRI translation award, Prof Morgan, Dr Zelek and colleagues in Oxford aim to progress development of a small molecule inhibitor that they have identified to target complement in the brain, while continuing to analyse new hits arising from his ongoing drug screens. The successful development of a brain-penetrant therapeutic against complement could offer a game-changing new approach to dementia therapy.
The UK DRI translational awards are possible though funding received from Alzheimer’s Research UK’s and UK Research and Innovation’s (UKRI) Impact Acceleration Account (IAA).
Article published: 30 October 2023
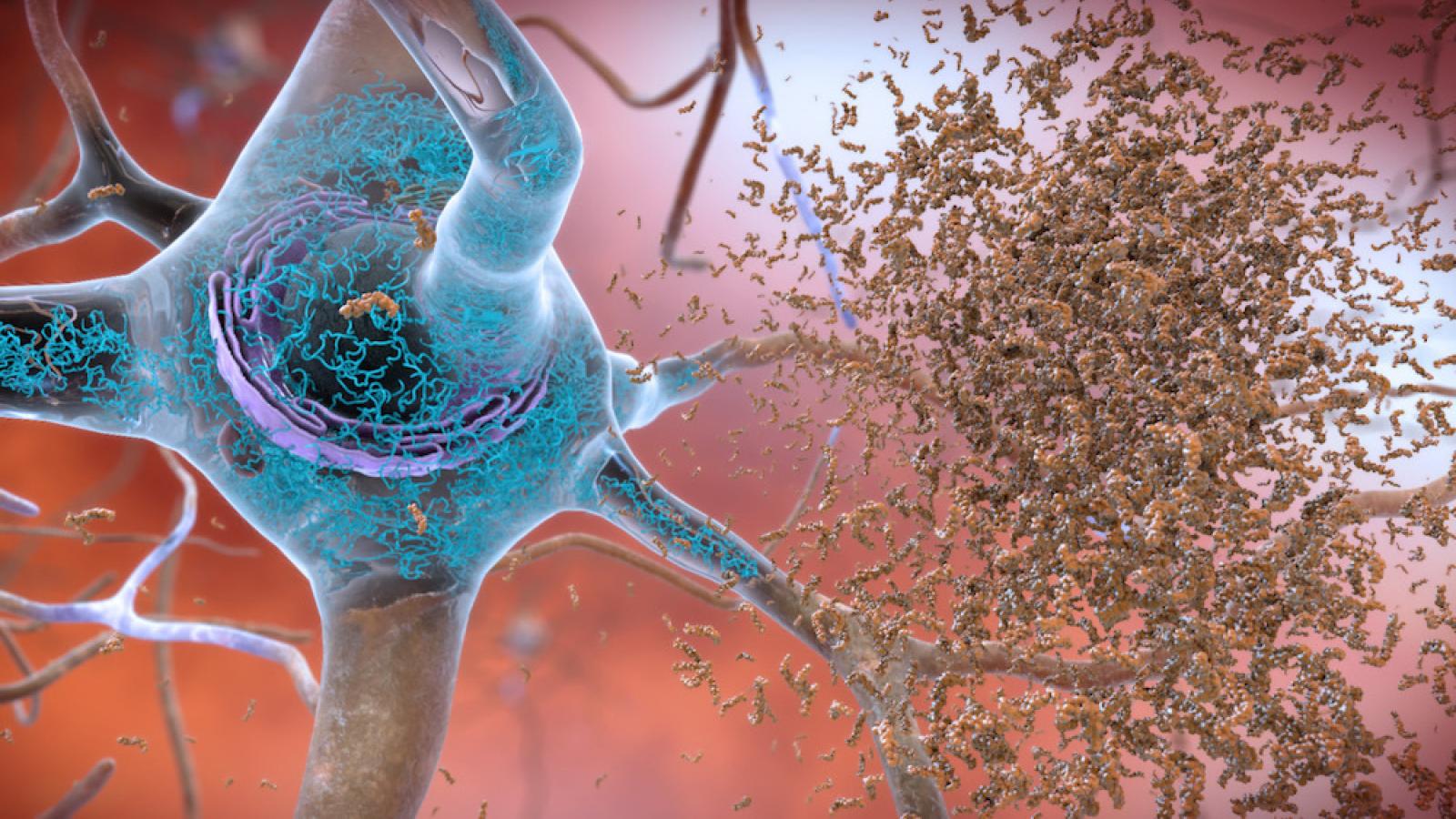
Banner image courtesy of National Institute on Aging, National Institutes of Health, U.S. Department of Health and Human Services.
projects funded in this latest translation award round