Biography
Professor Sir David Klenerman is a physical chemist who graduated and completed his doctorate at Cambridge University working with Professor Ian Smith on infra-red chemiluminescence for his PhD in 1985. This was followed by postdoctoral research at Stanford University, California with Professor Dick Zare on high overtone chemistry. He then returned to the UK and worked for seven years for BP Research in their Laser Spectroscopy Group before returning to the Department of Chemistry, University of Cambridge, progressing to a Professorship. At Cambridge his work has focussed on the development and application of physical methods, particularly laser spectroscopy and single molecule fluorescence, to biological and biomedical problems.
His recognition includes being knighted by the Queen in 2018, for development of high speed DNA sequencing, and being awarded the Royal Society’s Royal Medal in 2018. He was awarded the 2020 Millennium Technology Prize jointly with Shankar Balasubramanian and the 2022 Breakthrough Prize for Life Sciences and 2024 Gairdner Prize for Life Sciences jointly with Shankar Balasubramanian and Pascal Mayer for next generation DNA sequencing.
Klenerman Lab
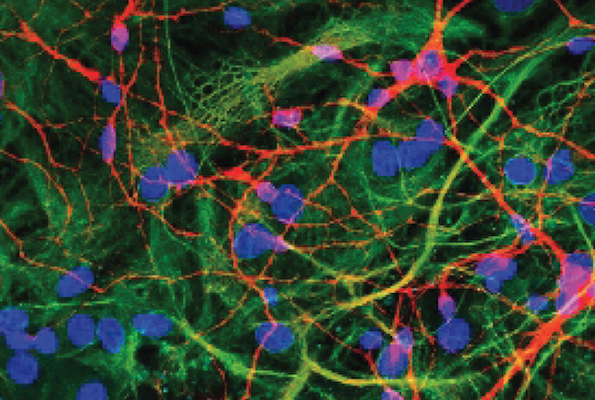
Explore the work of the Klenerman Lab focused on determining how protein clumps form, damage the brain and change as the different neurodegenerative diseases develop to know which ones to target for therapies.